Where you live can have significant impacts on your oral health.
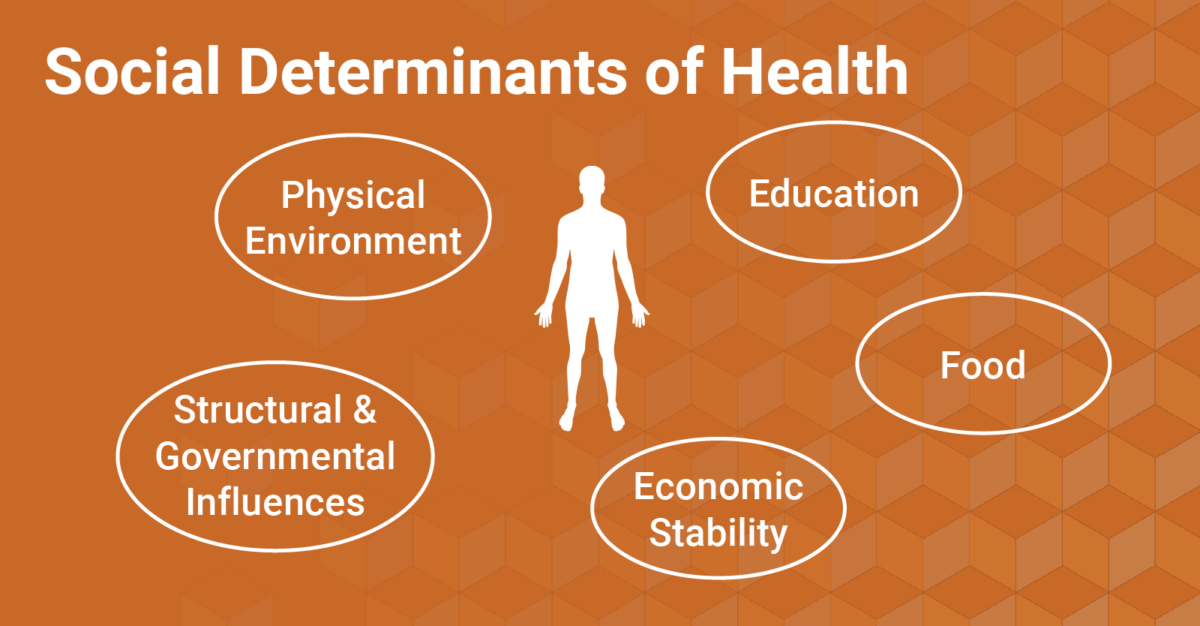
NCOHC recently dove deep into the first of a series of factors that impact health, known as “social determinants of health.” You can catch up and learn how government structures impact our oral health here.
A US National Resource Council and US Institute of Medicine report highlights three important physical environmental factors that impact health: proximity to toxic substances, like air pollution; access to resources, like grocery stores and health care practices; and community design, or the built environment.
All of these factors can have negative oral health consequences, from cavities and gum disease to tooth loss and oral cancer.
Can Pollution Really Impact Oral Health?
A study in the Journal of Clinical Pediatric Dentistry found that hard dental tissue could be an environmental indicator—your teeth can say a lot about the world around you. Children in this study living in high-pollution areas had higher cavity rates and even had significant levels of toxic compounds in their tooth tissues.
Similarly, a study in the British Medical Journal found an association between air pollution and mouth cancer.
These studies were conducted in the Eastern European country of Georgia and Taiwan, respectively. Georgia and other USSR countries endured significant environmental degradation during the Soviet era, and Taiwan is known to have particularly significant periods of air pollution.
While more research is necessary to explore links between pollution and oral health, one thing can be said for North Carolinians: if you live in a high-pollution area—such as in the vicinity of one of the 3,300 hog waste lagoons in the state—you are more likely to be Black and poor, two well-documented determinants of oral health.
Access to Resources and the Built Environment
In North Carolina, where you live can significantly impact your access to resources necessary to live a healthy life. For example, rural North Carolinians are more likely to live in food deserts. Poor nutrition and high intake of fast food and other high-sugar, high-carb foods significantly increases the risk of tooth decay and gum disease.
Additionally, 75 of North Carolina’s 100 counties are designated dental health provider shortage areas (dHPSAs). So, rural North Carolinians are more likely to face long drives—and in turn, longer periods of time off from work, childcare costs, and transportation costs—just to get to see a dentist.
To compound the effects of limited resources in rural areas, especially for low-income residents, other aspects of our built environment such as public transportation can further limit access to oral health care. In a city, you’re more likely to be able to hop on a bus if you need to see a dentist and don’t own a car. For much of rural North Carolina, however, that is simply not an option.
This isn’t to say that the only shortages in optimal oral health care occur in rural areas. There are plenty of urban food deserts, and oral health disparities between affluent and low-income individuals exist everywhere.
As we navigate oral health care systems and work to build an equitable future, where all North Carolinians have access to quality care, we have to think outside of the dental office. Join NCOHC in its work toward structural changes that expand oral health care access for underserved populations across our state.
To learn more and get involved, be sure to sign up for NCOHC news.
NCOHC is a program of the Foundation for Health Leadership & Innovation. For more information and to stay up to date, subscribe to the NCOHC newsletter. If you are interested in becoming an NCOHC member, you can also fill out our membership form. It’s free!