Last week, FHLI’s North Carolina Oral Health Collaborative attended the UNC Adams School of Dentistry’s Teledentistry Symposium, co-sponsored by the ECU School of Dental Medicine. Speakers from across the state joined oral health professionals in Chapel Hill to discuss technological innovations in oral health care and how they can be implemented to increase access across North Carolina.
The summit featured keynotes from experts in teledentistry as well as live demonstrations of the technology in action.
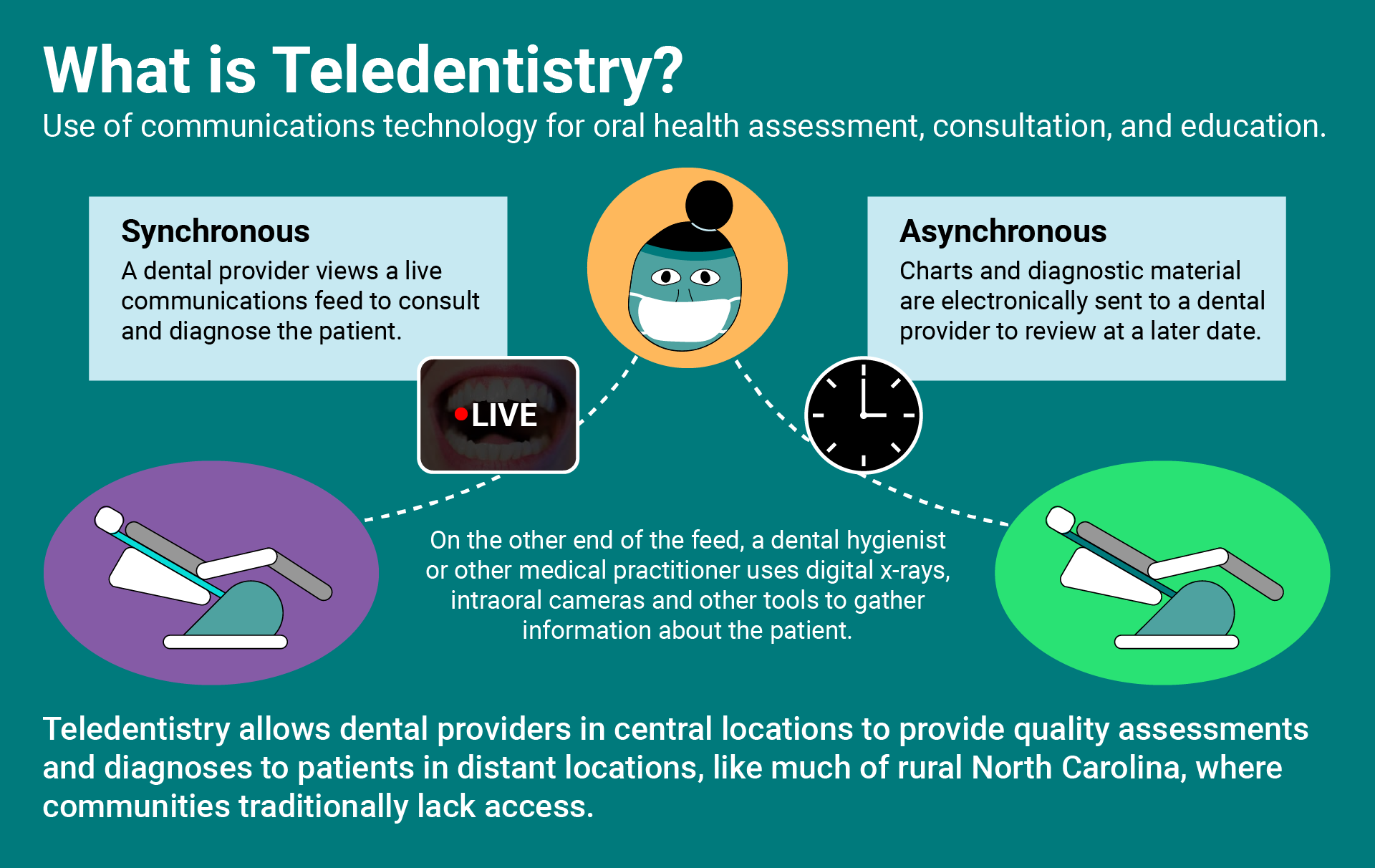
Dr. Rob Tempel and Dr. Andres Flores kicked off the demonstrations with a synchronous teledentistry consultation, followed by an example of asynchronous teledentistry from Dr. Shaun Matthews, the director of telehealth at UNC’s Adams School of Dentistry.

The 2020 Teledentistry Symposium follows UNC’s first ever Teledentistry Summit, which was held in October 2019. During his keynote address, Dr. Matthews reviewed the first summit and its goals, noting that oral health leaders have been successful in reaching those goals, including updating state-level dental hygiene regulations, visiting active teledentistry sites, and convening a statewide workgroup.

Dr. Shaun Matthews, director of telehealth at the UNC Adams School of Dentistry, giving his keynote address at the symposium.
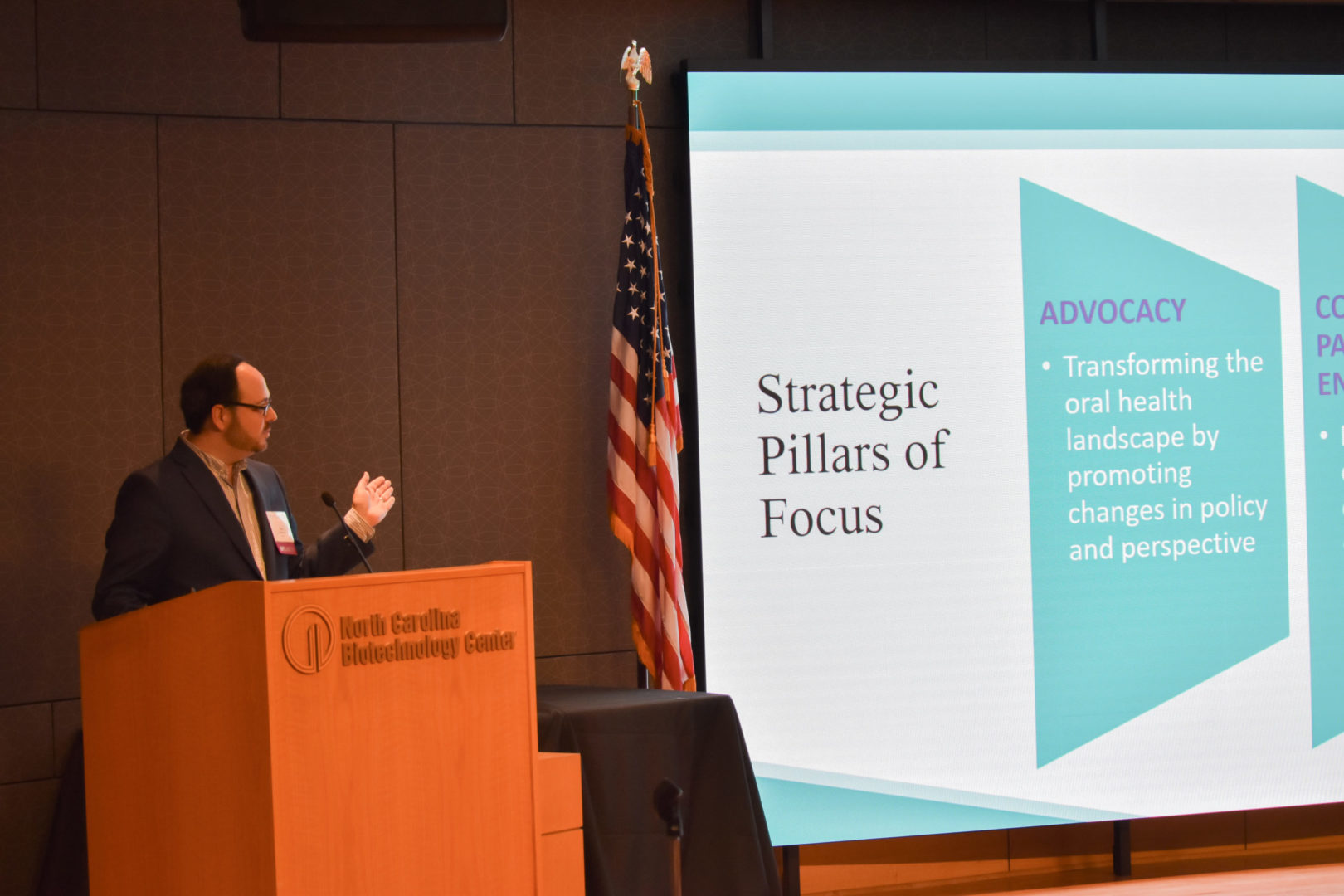
NCOHC Director Dr. Zachary Brian also gave a keynote address, discussing the use of teledentistry as a tool to increase access for underserved communities and the policy changes necessary to make that happen.
Here are some highlights and takeaways from the day:
1. Rural North Carolinians Disproportionately Lack Access to Oral Health Care
Of North Carolina’s 100 counties, 74 are designated Dental Health Provider Shortage Areas (HPSAs). Dr. Brian discussed how this landscape leaves residents in most of the state with limited access to in-person oral health care. This barrier is further compounded when considering the disparities in access between those on Medicaid and those with private insurance.

Dr. Zachary Brian discussing NCOHC’s role in addressing access gaps and barriers during his keynote address.
Dr. Sy Saeed compared oral health care disparities to access gaps and barriers in psychiatry, highlighting legislative efforts to promote telepsychiatry across the state. Compared to the 74-county oral health care shortage, a whopping 90 counties are psychiatric HPSAs. In an effort to combat the access gaps and to reduce emergency department visits, the state legislature passed a law in 2013 to create NCSTeP, a statewide telepsychiatry program.
2. We Have a Growing Shortage of Dentists
Dr. Brian discussed how a decline in our state’s dentist population is compounding the access issues facing rural North Carolinians. Dentists are retiring at a faster rate than they are graduating and beginning to practice. More troubling still, this shortage is only expected to increase through 2025.
Meanwhile, North Carolina’s dental hygiene programs are consistently at or near capacity, so we are simultaneously experiencing a hygienist surplus. This could be a promising trend, but North Carolina’s regulatory landscape restricts hygienists’ ability to practice at the top of their licensure. Additionally, dentists in North Carolina can only supervise two hygienists. So even with the growing number of practicing dental hygienists, the dentist shortage limits the workforce’s ability to expand access to crucial preventive services.
A panel of students discussed their perspective on the dentist shortage, disparities, and the use of technology to bridge coverage gaps. Student groups at UNC and ECU have formed to advocate for curriculum changes to incorporate teledentistry so graduating dentists are better prepared to positively impact oral health outcomes in North Carolina through technology.
3. Teledentistry Can Expand Access
All summit speakers agreed that connecting dentists in central locations with hygienists and patients across the state is an effective path to expanding access to traditionally underserved communities.
With teledentistry, dentists can remotely provide diagnostics measures like exams, assessments, consultations, and direct education to patients. Dr. Brian noted that almost all oral health issues are preventable, so increasing access to preventive care is a high-impact, cost-effective strategy to improving overall oral health outcomes.
In his address to the symposium’s attendees, ECU School of Dental Medicine Dean Greg Chadwick said that, “teledentistry is a tool, not a goal.”
The goal is expanded access, covering North Carolinians equitably. Innovation in teledentistry is a promising way to achieve that goal.
4. Significant Barriers Still Prevent Teledentistry from Expanding
While North Carolina law doesn’t prevent the use of teledentistry, there is currently no reimbursement model for Medicaid patients to receive asynchronous teledental care, and the payment rate for synchronous teledentistry is prohibitively low.
Dr. Mark Casey, NC Medicaid’s dental director, joined a panel of health care providers to discuss payment models to ensure providers are reimbursed for their services. All panelists agreed that payment parity is necessary, and they said that asynchronous reimbursement should be a top priority moving forward.
To get there, Bobby White, the CEO of the North Carolina Board of Dental Examiners (NCBDE), said that the NCSBDE is willing and anxious to move forward with teledentistry, but out-of-date language in the Dental Practice Act needs to be updated by statutory change.

From left to right: Dr. Alec Parker, executive director of the North Carolina Dental Society; Sommer Wisher, past president of the North Carolina Dental Hygienists’ Association; Bobby White, CEO of the North Carolina State Board of Dental Examiners and Greg Chadwick, dean of the ECU School of Dental Medicine.
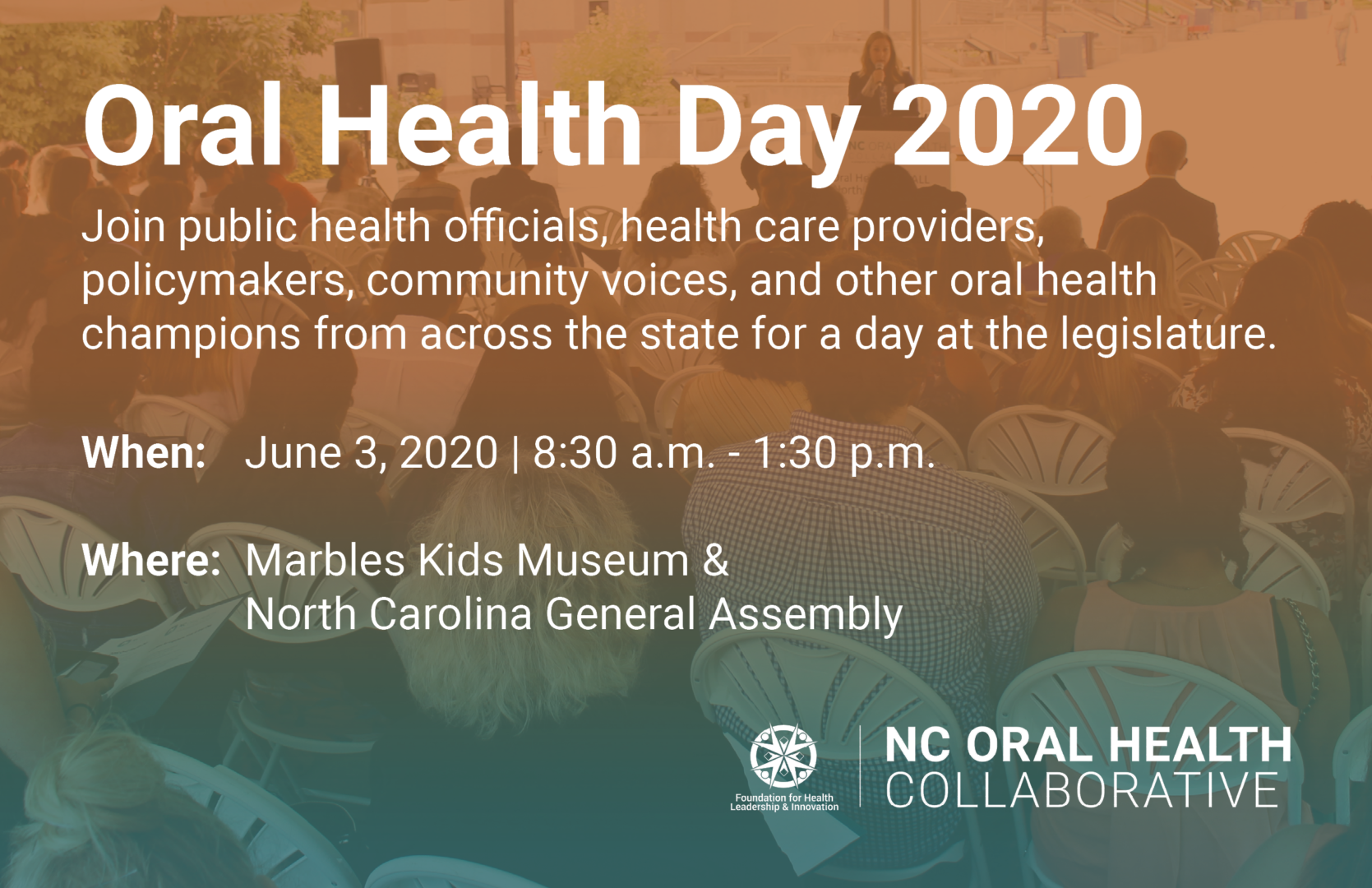
That’s why this year, NCOHC is dedicating its signature advocacy event, Oral Health Day 2020, to teledentistry.
On June 3, oral health professionals, community voices, and other oral health champions will convene at the North Carolina Legislature for a day of action and advocacy. We will engage and educate elected officials about the importance of teledentistry and the necessary legislative changes to allow it to expand into our state’s rural communities.
To learn more, visit our Oral Health Day 2020 page and register today!

To learn more and get involved, visit our Oral Health Day 2020 page to see what we are planning for our signature advocacy event on June 3rd . If you’d like to receive updates on stories like this directly to your inbox, be sure to sign up for NCOHC news.
NCOHC is a program of the Foundation for Health Leadership & Innovation. For more information and to stay up to date, subscribe to the NCOHC newsletter. If you are interested in becoming an NCOHC member, you can also fill out our membership form. It’s free!










 العربية
العربية 简体中文
简体中文 English
English Filipino
Filipino Français
Français Deutsch
Deutsch हिन्दी
हिन्दी Hmong
Hmong 한국어
한국어 Русский
Русский Español
Español தமிழ்
தமிழ் తెలుగు
తెలుగు Українська
Українська Tiếng Việt
Tiếng Việt