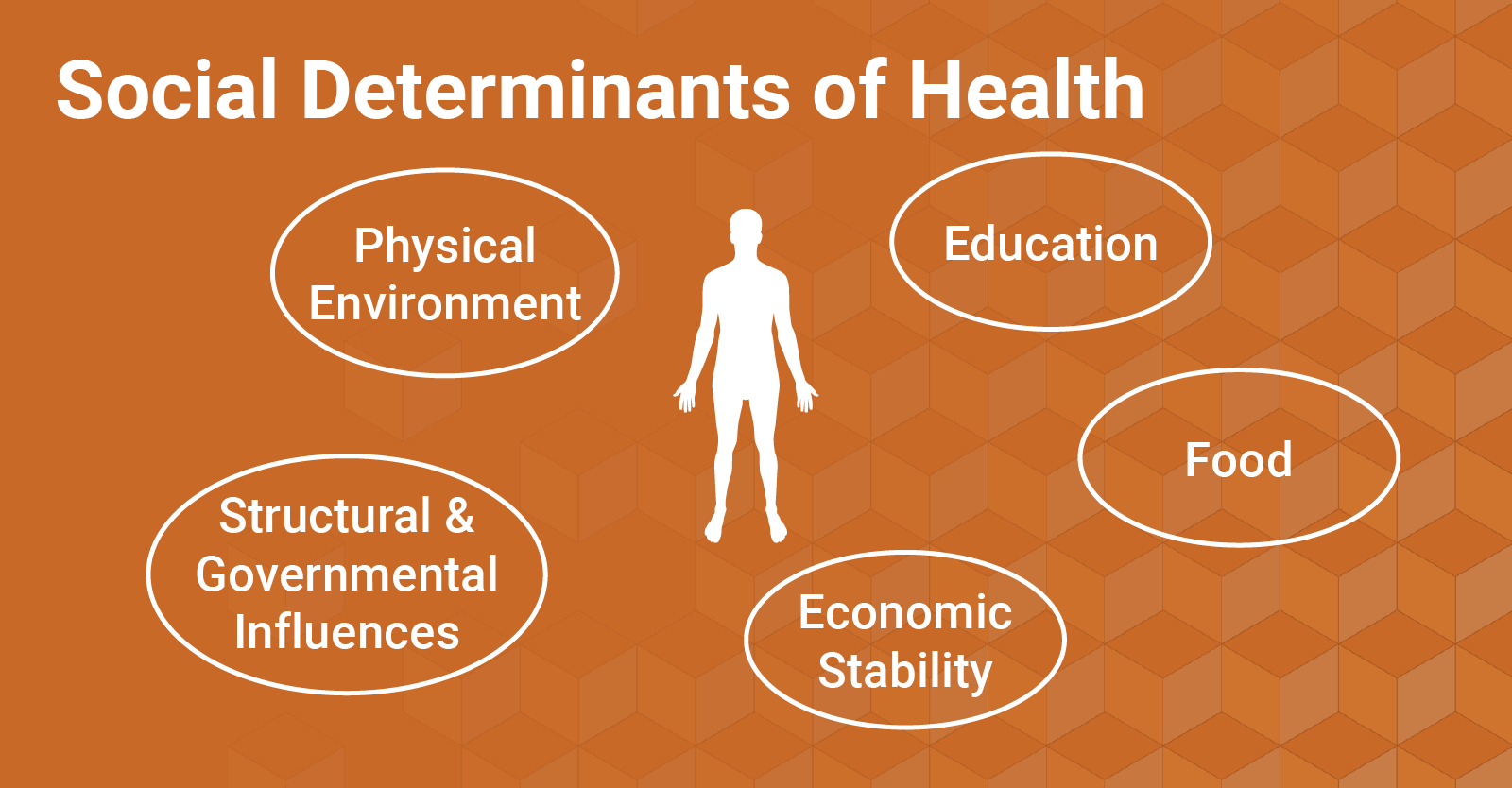
The heart of oral health equity is a blend of improving actual health care delivery, modifying public policy, and influencing structural change. Approximately 80 percent of a person’s health is the result of factors outside the doctor’s office, so it is necessary to account for all three. Each plays an important role in addressing systemic barriers to oral health care access.
We recently published an introduction to social determinants of health—the environmental conditions that impact a person’s health—outlining several categories of systemic barriers that prevent people from achieving optimal oral health.
From the physical distance between a patient and provider to the policy that governs dental practice, this week we’re diving into structural and governmental influences to see how they impact oral health outcomes.
Where can I go to access oral health care?
Depending on where you live, this can be a difficult question to answer. North Carolina ranks 37th in dentists per capita, with just 49 practicing dentists for every 100,000 residents.
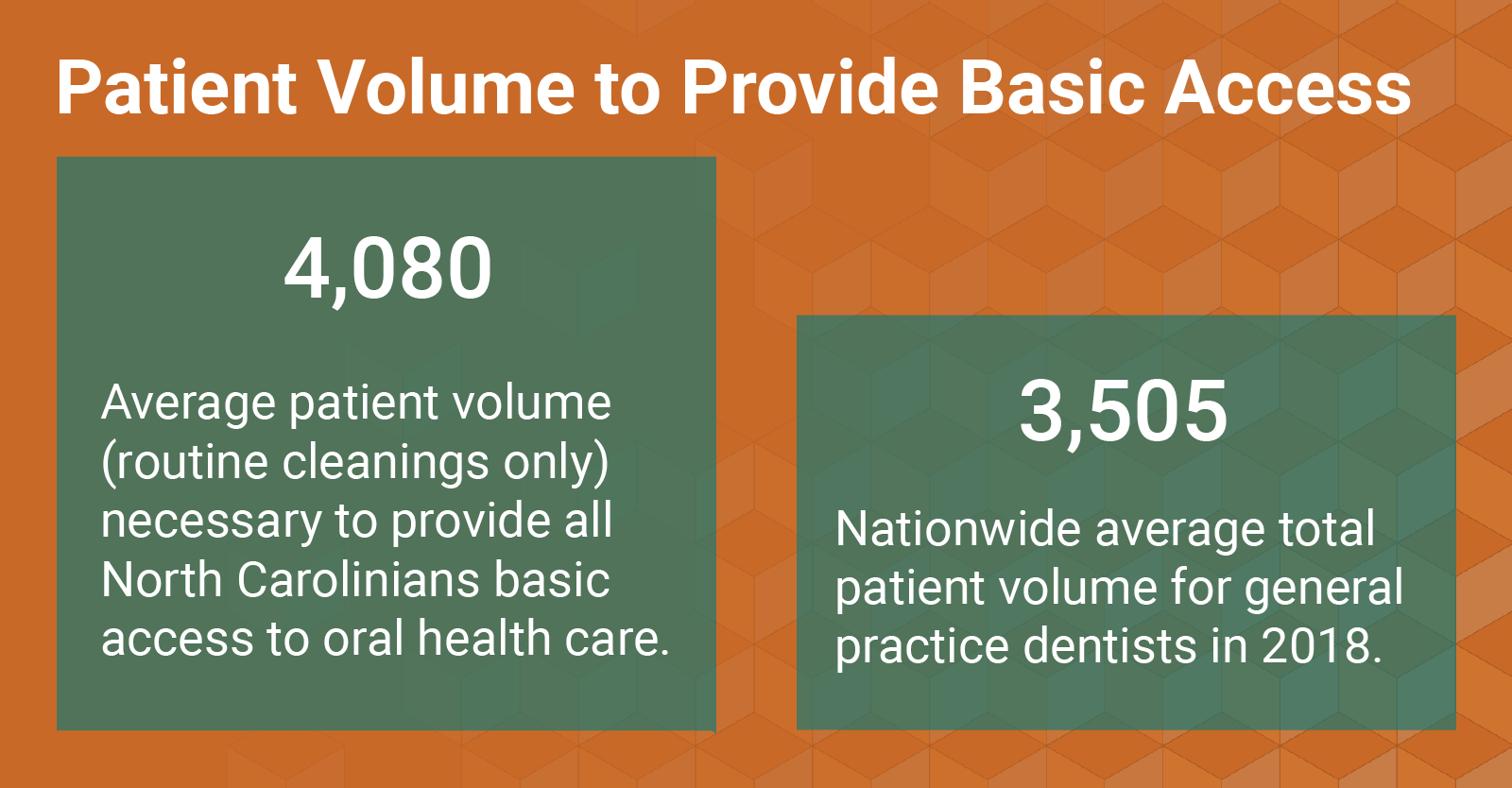
To put that in context, if all North Carolinians were to receive standard cleanings and check-ups every six months, every single practicing dentist in the state would need to field 4,080 appointments every year. And that doesn’t even account for emergency visits, restorations, and other care beyond regular preventive appointments.
Most of North Carolina’s practicing dentists are consolidated in just one fifth of the state’s 100 counties, compounding this shortage in rural communities. Seventy-four, predominately rural, counties are designated dental Health Provider Shortage Areas (HPSAs).
For many in North Carolina, the answer to, “Where can I go to access oral health care?” includes additional childcare, time off from work or school, and long drives (if they have access to a vehicle).
How do I pay for oral health care?
Even if every person in North Carolina could afford to see a dentist, it is clear from the statistics above that there isn’t the infrastructure in place to meet that demand. Everyone can’t afford to see a dentist, though. Oral health care is prohibitively expensive for many, especially those without insurance.
Many private practice dentists in North Carolina don’t accept Medicaid. However, for the uninsured and those on Medicaid, there is a great network of public health providers across the state. These clinics accept Medicaid and offer care on a sliding fee scale for those without insurance or who can’t afford to pay. Specifically, Federally Qualified Health Centers, local health departments, free and charitable clinics, among other entities across the state, offer these care options for those who lack access.
Unfortunately, the existing network of public health providers still doesn’t meet demand. Many patients simply aren’t familiar with what options are available in their communities, and those with urgent oral health needs often seek care in a hospital’s emergency department.
Emergency department physicians are not dental health professionals, so patients won’t get the needed treatments such as root canals, extractions or fillings when they go in for toothaches. Generally, an emergency department patient will receive a prescription for an antibiotic and an opiate, which will just calm the pain until the meds run out.
North Carolinians visit emergency departments at twice the national rate, and operating room costs for dental procedures exceed $40 million annually.
Increasing Visibility of Safety-Net Access Options During COVID-19
To help reduce emergency department demand for urgent oral health concerns during COVID-19, NCOHC has published an interactive map of oral health care safety nets across the state. The map is meant to serve as a tool to divert patients with urgent needs from emergency departments to nearby local health departments, Federally Qualified Health Centers, free and charitable clinics, and other safety nets.
The Collaborative is currently outlining strategies to re-purpose this map and develop additional tools that will help those with oral health needs find affordable care providers after the COVID-19 pandemic.

So, how do we change North Carolina’s oral health care structure to better meet the needs of those in our state?
The answer to this question in many ways lies in public policy. North Carolina is one of the four most restrictive states when it comes to allowing dental hygienists to practice to the full extent of their education and licensure.
While we have a serious, and growing shortage of dentists, we simultaneously have a growing surplus of dental hygienists. Unfortunately, state law only allows a dentist to supervise two hygienists at a time, preventing the growing workforce from having the opportunity to expand access to care, especially in remote areas where the dentist shortages are the most severe.
Earlier this year, NCOHC and the North Carolina Dental Society co-sponsored a change to Rule 16W.0104 of the Dental Practice Act. This change allows public health dental hygienists in Dental Health Provider Shortage Areas (HPSAs) to practice in community-based settings such as schools and long-term care facilities based on a written standing order from the supervising dentist, in lieu of a physically present dentist on site.
In one of our recent interviews, dental hygienist, educator, and advocate Crystal Adams said that if she could change anything in North Carolina’s regulatory framework, allowing dentists to supervise more than two hygienists would be at the top of her list.
There are many other policy proposals that could also increase access, like introducing postpartum Medicaid dental coverage, or modernizing the Dental Practice Act to allow providers to bill for telehealth care delivery.
Stay tuned as we break down other social determinants of health and the work being done to address them in the coming weeks.
Sign up for NCOHC’s newsletter list to receive updates on stories like this one directly to your inbox.
NCOHC is a program of the Foundation for Health Leadership & Innovation. For more information and to stay up to date, subscribe to the NCOHC newsletter. If you are interested in becoming an NCOHC member, you can also fill out our membership form. It’s free!