Dr. Kelly Bailey is a student at UNC-Chapel Hill pursuing a Master of Public Health degree. She has a unique perspective on the intersection between the environment and health, and this summer she worked with NCOHC to develop educational resources for dental professionals on issues related to PFAS contamination and cannabis legalization.
Can you tell me a bit about your career/education path prior to pursuing your current degree?
I graduated from the University of Florida with a bachelors degree in Microbiology and then went on to complete professional training at the University of Maryland School of Dentistry. I was incredibly fortunate to receive a scholarship through the U.S. Navy Health Professions Scholarship Program (HPSP). After graduating from dental school, I went on to serve in the military for eight years.
Where are you in school, what are you studying, and why did you choose that program?
I am currently entering my second year in the Master of Public Health (MPH) program at UNC Gillings School of Global Public Health, with a concentration in Environmental Health Solutions (EHS).
I chose the EHS concentration based on my interest in environmental justice, which is entangled in many of the “wicked issues” of our time, including oral health inequities. The environment and humanity are interdependent, and I think we are becoming increasingly aware of our connectedness to the natural world and to each other on a global level. We are all impacted by the environments in which we live, work, learn, and play, and I believe that a shift toward whole-person healthcare must incorporate environmental determinants of health to comprehensively address these pressing public health issues.
Where did you first hear about the North Carolina Oral Health Collaborative, and why did you want to pursue an internship with NCOHC?
During a dental health policy and management course, I had the pleasure of hearing Dr. Zachary Brian speak on barriers to dental care access in NC. It didn’t take much research on NCOHC afterwards to realize that their team is a small but mighty coalition of innovators and change-makers! NCOHC has been a leader in the advocacy space, fighting systemic barriers to dental care access through policy reform and education, and their group has catalyzed some really impactful changes in NC. Who wouldn’t want to be a part of that movement!?
What about public health dentistry is intriguing to you?
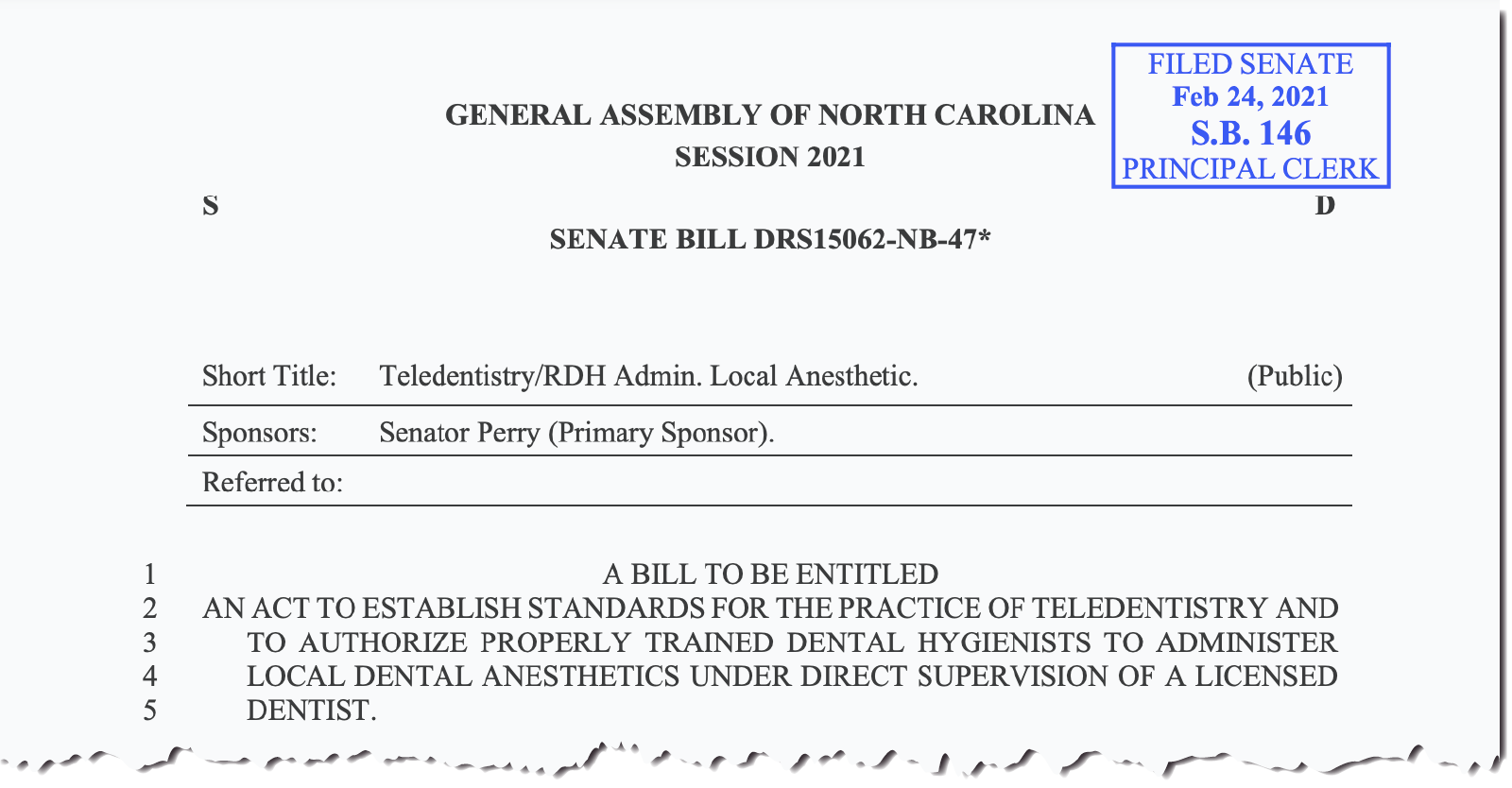
The dental public health (DPH) community is fundamental to leading the dental profession outside of its traditional silo and into integrated healthcare. From utilizing teledentistry services, to administering vaccines, to playing a role in natural disaster response, I think the profession’s scope of practice will continue to evolve in ways that foster multidisciplinary collaboration and improve the wellbeing of all North Carolinians. It’s an exciting time to be in DPH!
What’s a fun fact about yourself?
While overseas with the military, I traveled by ship to eight different countries and even lived in the beautiful country of Japan for two years. It was the experience of a lifetime for sure.
Tell me a bit about what you have worked on as an NCOHC intern. What do you hope to take away from the work you have been doing?
First, I was able to take a deeper dive into the PFAS contamination issue in North Carolina as it relates to oral and systemic health. Although this is a very well-publicized situation, I think there are certain connections that dental providers and dental public health professionals should be guided in making. PFAS contamination in drinking water is affecting most, if not all, of our patients, so we need to understand what we’re up against and what we can do as individuals and as a profession.
Secondly, I explored the topic of cannabis use in North Carolina. With several bills in legislation in NC, and legalization having been pushed through in VA, I think it’s really important to get clinical providers and public health professionals talking about cannabis use as it relates to patient health and the dental practice. There are still many unknowns about the long-term effects of cannabis use, but we already know a lot about cannabis-related racial stigmatization and it needs to be addressed within our community. The education we provide to patients should always be driven by a desire to heal, not to impose political beliefs.
If you could tell North Carolinians one thing you have learned that you think is important for everyone to know, what would that be?
Despite being largely preventable, oral conditions like dental caries and periodontal disease continue to threaten the overall health of too many North Carolinians, with disparate access to oral care services being one driver of this “silent epidemic.” For those who want to learn more, NCOHC is doing a lot of work in this area and has reader-friendly posts on their website. Also, Mary Otto’s book, “Teeth: The Story of Beautify, Inequality, and the Struggle for Oral Health in America,” is a great reference for better understanding the issues.
Denial of, or ignorance about, oral health inequities is still pervasive, and the dental community is not immune to this occurrence. I think this sums it up nicely and is a good reminder to all of us:
“When we’re not hungry for justice, it’s usually because we’re too full with privilege.” – Carlos A. Rodriguez
What’s next for you?
I will be applying to the DPH residency program, based in the NCDHHS Oral Health Section, in hopes of joining the phenomenal community of DPH researchers, academics, and leadership professionals. Ultimately, I’m hoping to apply my skills within a community-based organization or at the state level.