The North Carolina Oral Health Collaborative (NCOHC) recently released its first policy brief. The document outlines changes to North Carolina’s regulatory framework that, if enacted, could significantly increase access and equity in oral health care.
In the coming weeks, NCOHC will publish a series of deep dives into each section of the policy brief to explain the details of each proposal and how each could improve care for underserved North Carolinians.
North Carolina’s oral health workforce faces a growing imbalance that unnecessarily restricts access to care. The dental hygienist workforce is growing, and North Carolina’s dental hygiene programs remain competitive and full. Unfortunately, the population of practicing dentists is shrinking as dentists age out and retire faster than new ones graduate and enter the workforce.
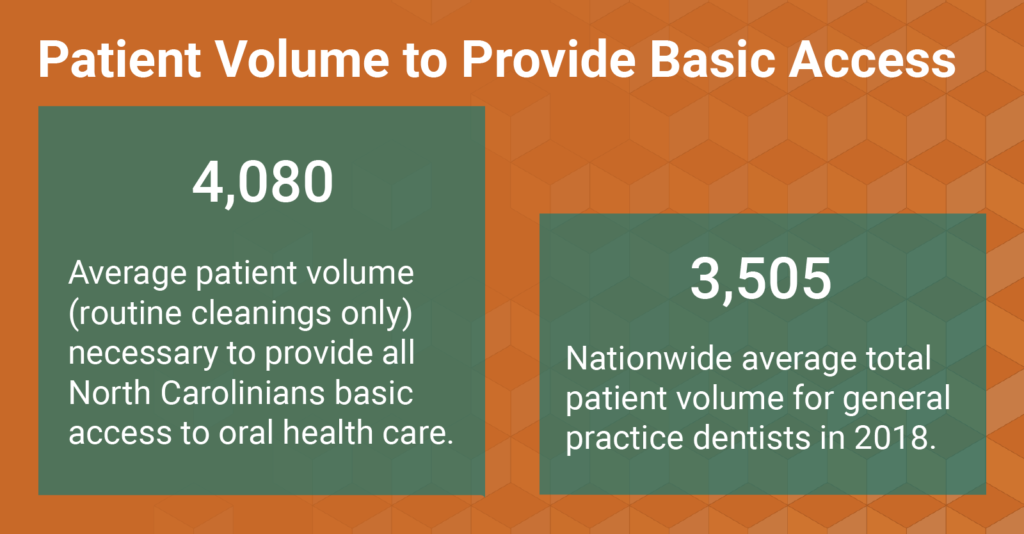
This is a serious concern, as many of the access gaps in North Carolina are driven by a lack of dentists in rural and already underserved areas. In a recent post, NCOHC found that every practicing dentist in North Carolina would need to see 4,080 patients every year just to provide all residents with standard cleanings and checkups, not including follow-up appointments or visits for fillings and other advanced procedures.
With these trends in mind, it is important that North Carolina leaders take steps to allow the oral health workforce to provide care more efficiently. The proposals in the Workforce Utilization section of our policy brief address five policy changes* that can help:
- Revise the two hygienist per dentist supervision ratio
- Revise supervision definitions, primarily looking at revision of “direct supervision”
- Expand delegated duties for hygienists
- Eliminate restrictions on hygienists’ delivery of local anesthesia
- Recognize and credential Expanded Function Dental Assistants (EFDAs)
*It is important to note that these proposals do not necessarily reflect NCOHC’s current policy priorities. Rather, they are evidence-based steps that, if implemented, would increase access and equity in oral health care for North Carolinians across the state.
Supervision Requirements
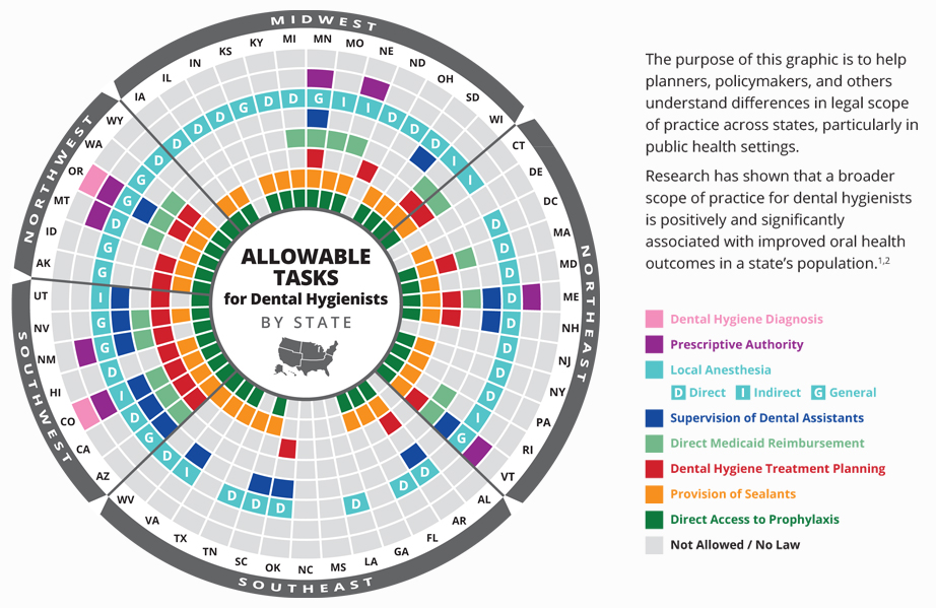
North Carolina is considered one of the more restrictive states for dental hygiene scope of practice parameters. The North Carolina Dental Hygiene Act restricts dentists in private practice from employing more than two dental hygienists at the same time, and it also requires direct supervision—the most stringent form of supervision in a dental office—for most tasks that hygienists are effectively trained to perform.
Easing restrictions to these supervision requirements could significantly increase care provided, especially in community-based settings like school-based clinics and long-term care facilities, where dentists may not always be available on site.

Source: North Carolina General Statutes Chapter 16
Fortunately, easing direct supervision requirements, and expanding the number of hygienists a dentist can supervise, are not new or unique approaches to expanding access and equity in care delivery. Many states across the country have taken these steps, and often these changes were enacted several years ago.
Earlier this year, North Carolina took one important step toward a more equitable oral health landscape by allowing public health hygienists to work outside of direct supervision and rather based on a written standing order from the supervising dentist. The 16W rule change was important, but it only applies in limited settings. Allowing the rest of the dental hygiene workforce to practice in similar settings by written standing order instead of with a dentist physically present on site could significantly increase how many North Carolinians receive basic screening and preventive dental services.
Revision of Delegated Duties
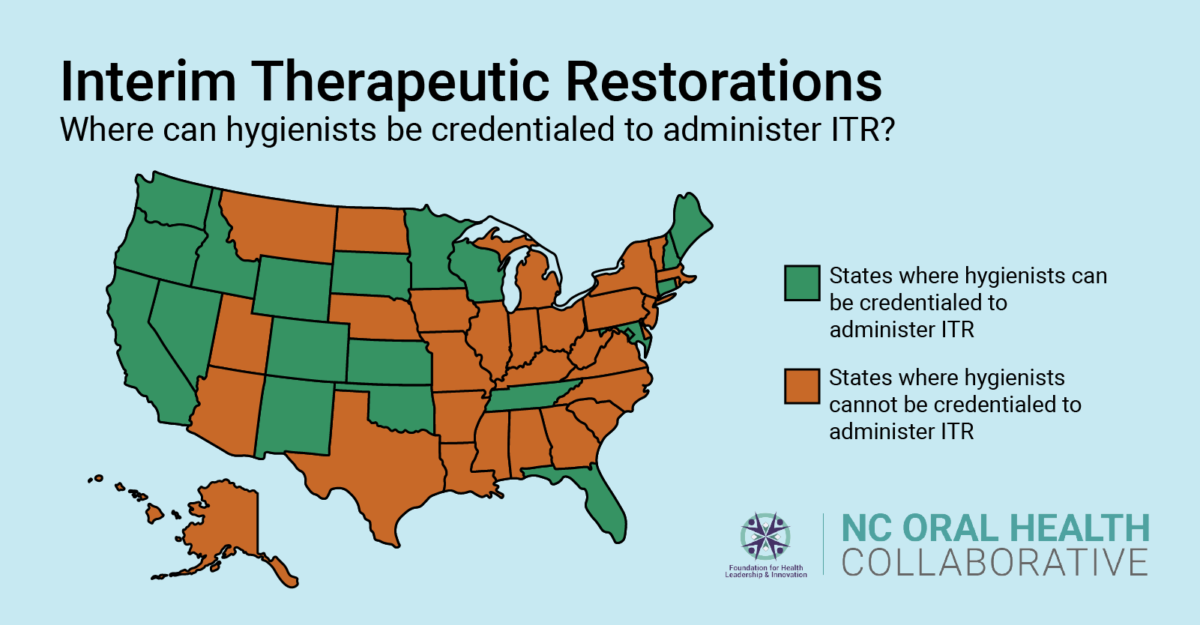
North Carolina’s regulatory framework prevents hygienists from performing several clinical services in which they are required to be learn in their dental hygiene programs. With a few updates to include duties commonly delegated to hygienists in other states across the country, hygienists could significantly improve care access to the underserved, especially in settings outside the traditional dental office.
Source: oralhealthworkforce.org
The NCOHC policy brief’s proposals for additional duties for hygienists includes interim therapeutic restorations (ITR), which refers to a restoration placed on a tooth to prevent the progression of a cavity. ITR’s should be done only in specific cases, when the cavity or decay in question hasn’t progressed too far. You can further read about ITR’s in the American Academy of Pediatric Dentistry’s Policy Statement on their use.
ITR is proven to reduce levels of cavity-causing bacteria and is used mostly when treating children and infants, especially when full restorative care is unavailable, unaffordable, or needs to be deferred.
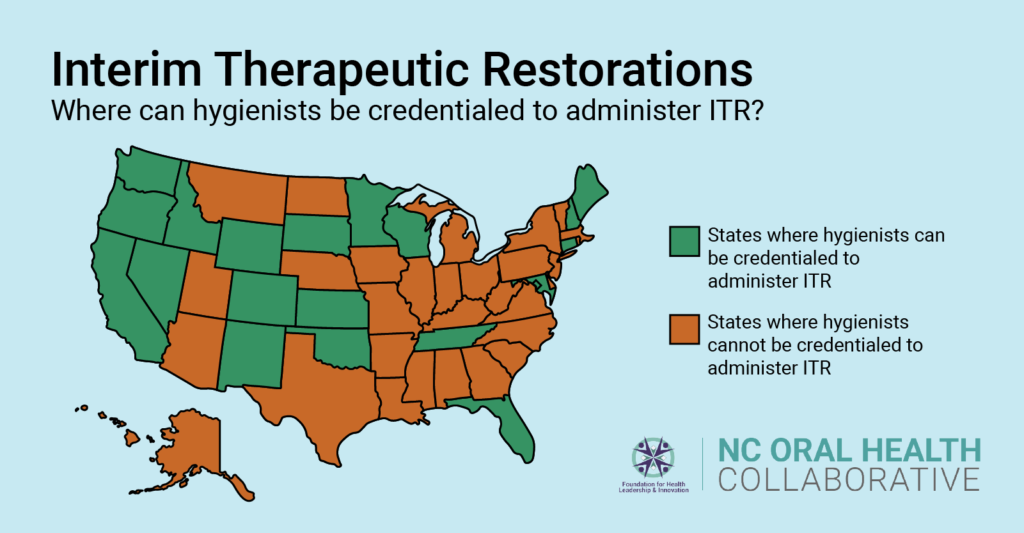
Source: ADHA
When restorations or other surgical procedures are necessary, dental hygienists could improve efficiency in the dental office by administering local anesthesia, which they are provided the didactic training for in their dental hygiene programs but prevented from performing under North Carolina law.
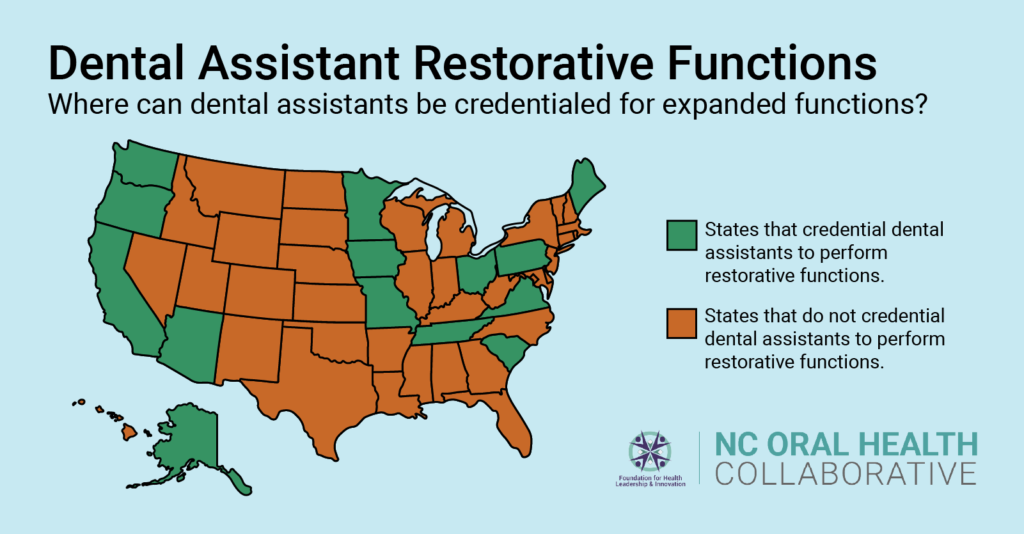
Along with hygienists, dental assistants play important roles in the dental office, and they, too, could increase dental office efficiency if allowed to perform expanded functions. Many states credential Expanded Function Dental Assistants (EFDAs). This workforce receives additional training to perform certain restorative procedures, such as the direct placement and modification of restorative filling material.
Source: AAPD
Stay tuned as we break down the rest of NCOHC’s policy brief. To receive updates in your inbox, sign up for NCOHC news today!
NCOHC is a program of the Foundation for Health Leadership & Innovation. For more information and to stay up to date, subscribe to the NCOHC newsletter. If you are interested in becoming an NCOHC member, you can also fill out our membership form. It’s free!