“Historic and systemic structural racism are inherent parts of the United States,” said Jen Zuckerman, director of strategic initiatives at the Duke World Food Policy Center. “This means every single system that exists within the United States is rooted, designed, and based in racism, and has been built on the system of oppression. Nobody alive today is to blame for the unfairness of our history, but we each hold a responsibility to create a better future.”
Continuing NCOHC’s series on the social determinants of health and how they impact equity in oral health, we spoke with Zuckerman to discuss how the Duke World Food Policy Center approaches inequities in food systems and the policy work that can make a lasting impact.
Click here for more on equity in oral health.
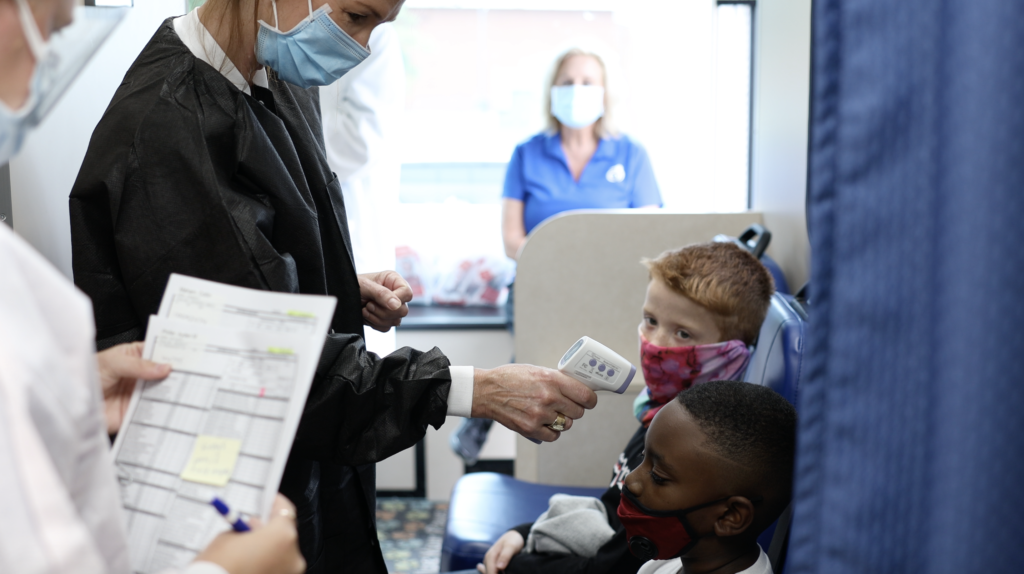
Access to food is an important social determinant of health, and healthy food options can significantly impact oral health. Unlike other posts in this series that directly break down relationships between the social determinants and oral health, this post will focus on food systems, underscoring how Zuckerman and the Duke World Food Policy Center are addressing inequities, while drawing parallels to oral health systems.
Lack of access to affordable, healthy food options means consumption of less healthy food, often high in sugar and carbohydrates. This is an important concern, as these kinds of foods increase risk of tooth decay, gum disease, and other oral health issues.
The Center for Assessment and Policy Development defines racial equity as “the condition that would be achieved if one’s racial identity no longer predicted, in a statistical sense, how one fares.”
Racial inequity plagues food production, distribution, financing, ownership, and access in the U.S., so much so that Zuckerman said there is no true working example of an equitable food system. To understand the fundamental role that racism plays in creating systems of inequity, the World Food Policy Center looks toward ownership structures.
“An equitable food community is one where there is an equitable distribution of ownership as it relates to the ability to grow food, distribute food, and provide retail,” Zukerman said. “An equitable food community would also have equitable access to capital.”
The Duke World Food Policy Center uses the term “Food Apartheid” to refer to areas with limited access to healthy food options. Food Apartheid broadens the conversation to include various factors and root causes of inequities in the food system such as historic disinvestment from communities of color.
The term “food desert” insinuates that the phenomenon is naturally occurring. Zuckerman pointed out that to truly understand the underlying structures that create food inequity, we must understand how points of limited access are influenced by generations of intentional disinvestment.
The ability — or lack thereof — to build generational wealth has been fundamental in creating inequities. According to the Duke World Food Policy Center, barriers to building generational wealth should also be front and center in policy work to address and reverse inequities.
“When we think about food, or when we think about anything in the United States, history has demonstrated that the white community has continually gotten investment through policies, programs, and initiatives,” said Zuckerman. “And communities of color have continually gotten programs and services, which do not build wealth.”
While programs and services for those who lack access are incredibly valuable, it is simultaneously important to take conversations of equity a step further to encompass the financial, policy, and power structures at play.
What does ownership look like in the oral health space? According to a 2015 ADA report, 74.2 percent of licensed dentists are White, while only 3.8 percent are Black, 5.2 percent are Hispanic, 15.7 percent are Asian, and 1.1 percent are other non-White ethnicities.
Zuckerman pointed to housing as an example of racist policies that have created lasting impacts on generational wealth. White veterans returning from World War II were able to buy homes through the GI bill, while returning Black veterans were disproportionately blocked from homeownership due to redlining and other policies rooted in racism.
“Broadly speaking, instead of home loans, Black veterans got public housing from government support,” said Zuckerman. While policies like redlining are illegal today, “think about the wealth built over generations of homeownership versus the wealth you cannot build by living in public housing.”
In North Carolina, the racial disparity among dentists is even wider. Around 82 percent of practicing dentists in North Carolina are white, according to a 2005 report from the UNC Sheps Center for Health Services Research. Which communities have been able to benefit most from generational wealth thanks to the dental industry, and which communities have not?
Racist policies, no matter when they were enacted or ended, have contributed to an historic disparity in wealth between white and BIPOC communities. Because of this, a lack of direct racism is not enough to reverse past racism. Whether we are aware of it or not, there are still people, policies, and structures in place today that have disproportionate negative impacts on communities of color.
So, how do we actually change racist systems and create equitable structures?
According to Zuckerman, ownership, which refers to both wealth creation and agenda setting, is a central piece of the puzzle.
“There need to be changes in financing and philanthropic investments,” Zuckerman said. “More philanthropic dollars need to be invested in BIPOC-led organizations, and those community organizations need to be able to set the agenda for what they would like their community to have.”
In oral health, significant focus is given to providing low-cost oral health services to those who have historically lacked access. While these programs and services are incredibly important, and this post is not in any way meant to downplay the hard work that so many people do to extend access, oral health champions can learn a lot from the Duke World Food Policy Center’s perspective.
As oral health policy champions, how can we help create more equitable structures that include a diverse workforce more representative of the population as a whole? Where is wealth being built in the dental industry, and how can we work to increase access to and equity in that side of the equation?