Parker Norman is an undergraduate student studying Health Policy and Management at the UNC Gillings School of Global Public Health with minors in Spanish and Entrepreneurship. As an NCOHC intern, Parker is researching dental care management workforce models with a focus on dental navigators and ADA-formalized Community Dental Health Coordinators.
The oral health care industry is beginning to face dramatic changes, like a focus on the social determinants of health, a shift to value-based care, more widespread use of teledentistry, and the employment of emerging oral health workforce models. New allied dental health professionals are becoming more common, especially as many of these models are better equipped to withstand the coming changes in the oral health care industry.
Dental care management workforce models focus on expanding access to oral health care through care coordination, especially for populations at greater risk of low oral health status and an inadequate or lack of oral health care access. Target populations may include those who are from low-income families, members of minority groups, those living in underserved areas, children, and/or the older adult population, among others. These models connect people with oral health services and the resources necessary to access those services. These resources include reliable transportation, comprehensive oral health insurance coverage and providers who accept that insurance, and providers who speak the same language as their patients.
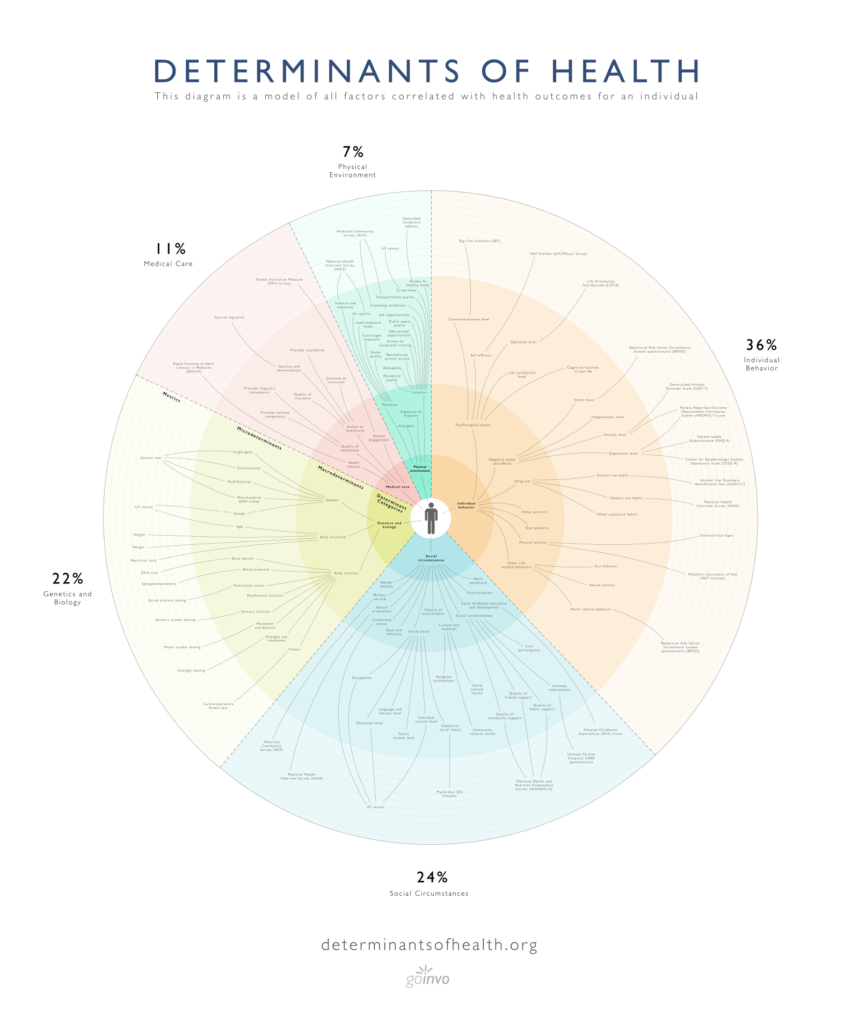
NCOHC recently highlighted the social determinants of health (SDOH) and how these non-medical drivers outside of direct clinical care can affect a person’s health. Social determinants broadly fit into five categories, including economic stability, education, social and community context, health and health care, and one’s neighborhood and built environment. Social determinants in each category may include:
- Economic Stability: employment; food insecurity; housing instability; poverty
- Education: quality childhood education; high school graduation; language and literacy
- Social and Community Context: discrimination; racism; social cohesion and support
- Health and Health Care: financial and geographic access to care; health literacy
- Neighborhood and Built Environment: access to foods that support healthy eating patterns; transportation options; environmental conditions; public safety
For more on the social determinants of health and to view supplemental information for the graphic above, visit determinantsofhealth.org
By addressing social determinants across each category, a person who may face multiple barriers is better equipped to achieve optimal overall health. Dental care management models offer an opportunity to address multiple determinants of oral health and improve overall access to oral health care by breaking down financial, geographic, and cultural barriers.
Types of dental care management workforce models that focus on expanding access to oral health care through care coordination include dental navigator models and the ADA-formalized Community Dental Health Coordinator model (CDHC). General dental navigator models include variable, on-site training programs that are tailored to the target populations they serve. With no specific prerequisite requirements, education before employment as a dental navigator may not be necessary, but on-site training does occur.
The CDHC model is an ADA-formalized model with a specific educational curriculum, training and internship requirements, and professional licensure requirements before employment. While the national curriculum is not geared towards target populations, a CDHC model may be adjusted for communities served. It also often takes longer for a CDHC to be able to be employed, given the formalized criteria that needs to be met first. However, once employed a CDHC is already equipped with education and training.
These models both aim to employ culturally competent individuals from the communities they serve, and who are better able to understand the needs of vulnerable target populations and connect them with the resources necessary to access optimal oral health. These individuals may speak the same language(s) as the communities they serve, which often helps the people in those communities feel more comfortable.
Along with improving access to care, dental navigators and CDHCs promote oral health literacy through patient education, often delivered in a patient’s native language. With an understanding of the importance of good oral health, people are more likely to seek and utilize oral health care. Thereby, these models not only improve access to oral health care but promote actual utilization of oral health care services.
Dental navigators and CDHCs are already employed in North Carolina. Crystal Adams, a registered dental hygienist and Director at Catawba Valley Community College’s Dental Hygiene Program, helps to oversee the education and training of CDHCs across the state. Dr. William (Bill) Donigan, Dental Director at Kintegra Health, has employed and trained dental navigators on-site over the last eight years.
An upcoming blog post will discuss outcomes of these models in North Carolina and how they are increasing access to oral health care. It will also highlight Adams’ and Donigan’s recommendations for our state as we put more of these models into practice. Dental care management models, including the dental navigator model and the CDHC model, are becoming increasingly more important to consider. By expanding access to dental care for vulnerable populations, oral health inequities can be addressed, and the oral health for all North Carolinians improved. Stay tuned, we will follow-up soon with more from Dr. Donigan and Crystal Adams, breaking down the similarities and differences of the CDHC and navigator models of care coordination.
NCOHC is a program of the Foundation for Health Leadership & Innovation. For more information and to stay up to date, subscribe to the NCOHC newsletter. If you are interested in becoming an NCOHC member, you can also fill out our membership form. It’s free!