We can acknowledge it. “Oral health policy advocacy” is not exactly something you hear every day, right? Imagine meeting new people at a party (fully vaccinated and masked, of course) and telling them, “I work in oral health. Not in a dental office, but in structural reform and policy advocacy.” You would get a few quizzical head tilts.
However, policy advocacy is incredibly important in our work to increase equity and access to oral health care. Plus, to effectively impact policy, those of us who are already engaged need to bring more people into the conversation. We need broad coalitions working for change to see better policy take hold, so it’s worth asking the question:
“So, how can policy impact my teeth?”
Let’s start by laying out the ways you can keep your mouth healthy.
First is hygiene. Maintaining healthy habits at home is the best way to prevent tooth decay and gum disease.
Next comes professional care. Everyone should see a dentist at a regular interval for a cleaning and checkup. That interval may vary for some, but usually, it is recommended that you see a dentist twice each year.
These seem like simple steps, but everyone has different levels of access to oral health resources, and different levels of understanding when it comes to good oral health habits.
So, how does policy fit in?
What if you don’t have dental insurance or don’t have transportation to get to the dentist? Or, what if you want to improve your habits, but are struggling to wade through mountains of misinformation to figure out if you should use fluoride toothpaste?
Under our current structure, good oral health relies in so many ways on variables that one may not always be able to control. That’s where policy reform can make a difference.
Take school-based care as an example. In underserved communities across North Carolina, dental programs that go into schools at regular intervals can provide children with the regular oral health care services they may not otherwise receive.
That care can help maintain good oral health during a child’s formative years, and it can help build healthy habits that last a lifetime. And in these settings, transportation and many other barriers are taken out of the equation.
Unfortunately, however, there remain policy barriers to expanding school-based access. School-based oral health programs rely heavily on dental hygienists, and North Carolina law can limit the type and how these services are delivered.
Many duties delegated to hygienists require a dentist to be physically present on site. Dentists generally need to be in their brick-and-mortar facility, limiting opportunities for hygienists to get out into community and provide care in settings like elementary schools.
Policy changes that allow hygienists to practice with in community-based settings — an opportunity with increasing validity given advances in teledentistry technology — and policy changes to increase the number of hygienists a dentist can supervise, among others, could significantly expand access to oral health care in non-traditional formats.
For example, a regulatory rule change in 2020 now allows public health hygienists in provider shortage areas to offer more services in non-traditional settings such as schools, without a prior exam from a dentist.
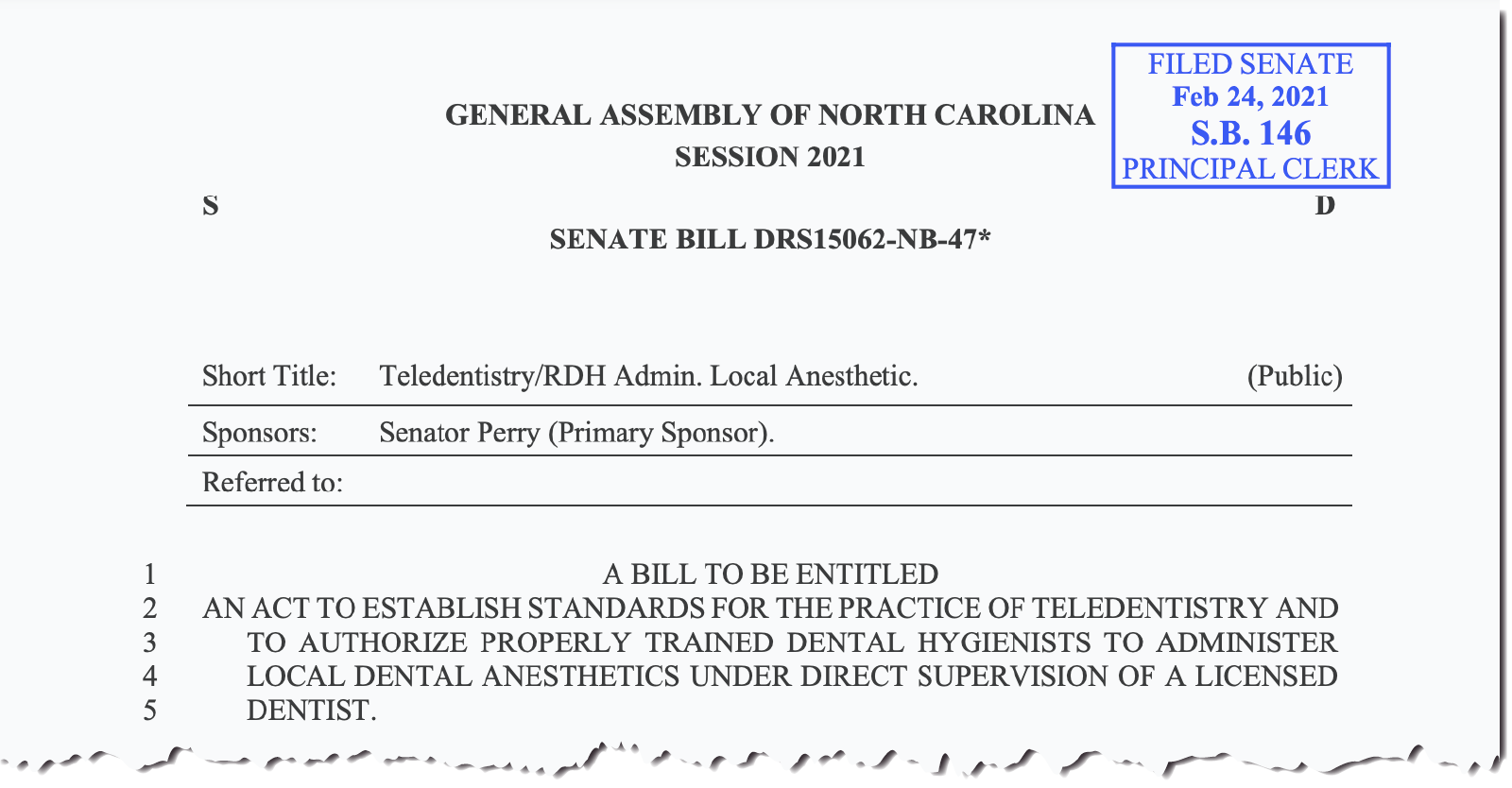
Policy can also increase efficiency in the dental office. Currently, legislation in the North Carolina General Assembly would allow dental hygienists to administer local anesthesia. This clinical function, which has already been delegated to hygienists in 44 other states and Washington D.C., would help practices increase efficiency, reduce costs, and care for more patients.
Note: Since this blog was published in July 2021, North Carolina Senate Bill 146 passed and was signed into law. You can find the enacted legislation here.
“But I have dental insurance and maintain good habits. Why should I care about policy?”
Proactive policy is not just a moral cause. Having more people experiencing good oral health is valuable in and of itself, but that reality carries positive impacts far beyond the individuals who are directly affected.
Treatments for preventable health conditions account for 75 percent of all health care spending in the U.S., and we only spend around 5 percent of health care dollars on preventive efforts. There is a huge opportunity to save money simply by boosting preventive efforts and warding off poor health conditions like tooth decay and gum disease before they can take hold.
What happens when someone with no insurance has a toothache? More often than not, that person will go to a hospital emergency department, where their pain may be managed but the source of the problem is not addressed. They may leave with a large hospital bill and likely another hospital visit in the near future if they are unable to seek care from a dentist.
If that individual can’t afford the hospital tab, the bill goes unpaid. Nationwide, uncompensated care costs add up to $42.4 billion every year. Nearly 80 percent of those dollars are eventually paid by taxpayers.
So, spending money up front to prevent poor health outcomes, both in our mouths and throughout our bodies, can significantly impact where our tax dollars go in the long run. Click here for more on the economics of preventive care.
NCOHC is a program of the Foundation for Health Leadership & Innovation. For more information and to stay up to date, subscribe to the NCOHC newsletter.



