The North Carolina Oral Health Collaborative’s parent organization, the Foundation for Health Leadership & Innovation, moved to remote work back in March. Social distancing can be a difficult transition, so we decided to check in on our co-workers, and their new office mates, to see how they’re doing.
Ava O., Foundation for Health Leadership & Innovation

Ava is tired after a very long day helping her mom at the office. She waits patiently but is delighted about the work-from-home situation. She has put in a formal request for more belly rub breaks during the workday.
Ava S., NCCARE360

Ava is frustrated that her office isn’t warmer, but she has found that sleeping on the job is a solution she can work with.
Blu, North Carolina Oral Health Collaborative

Blu has really stepped up to the plate since FHLI moved to remote work. He retains some sense of normalcy by dressing up for Zoom calls, and he loves screening emails in his outdoor office. He’s very glad to have so much company during the day.
Diesel, Center of Excellence for Integrated Care

Diesel is an older fellow. He just turned 11 in January. He’s grateful that his workmates moved their office to the first floor, so he doesn’t have to navigate the stairs.
Edie and Pearl, Practice Sights
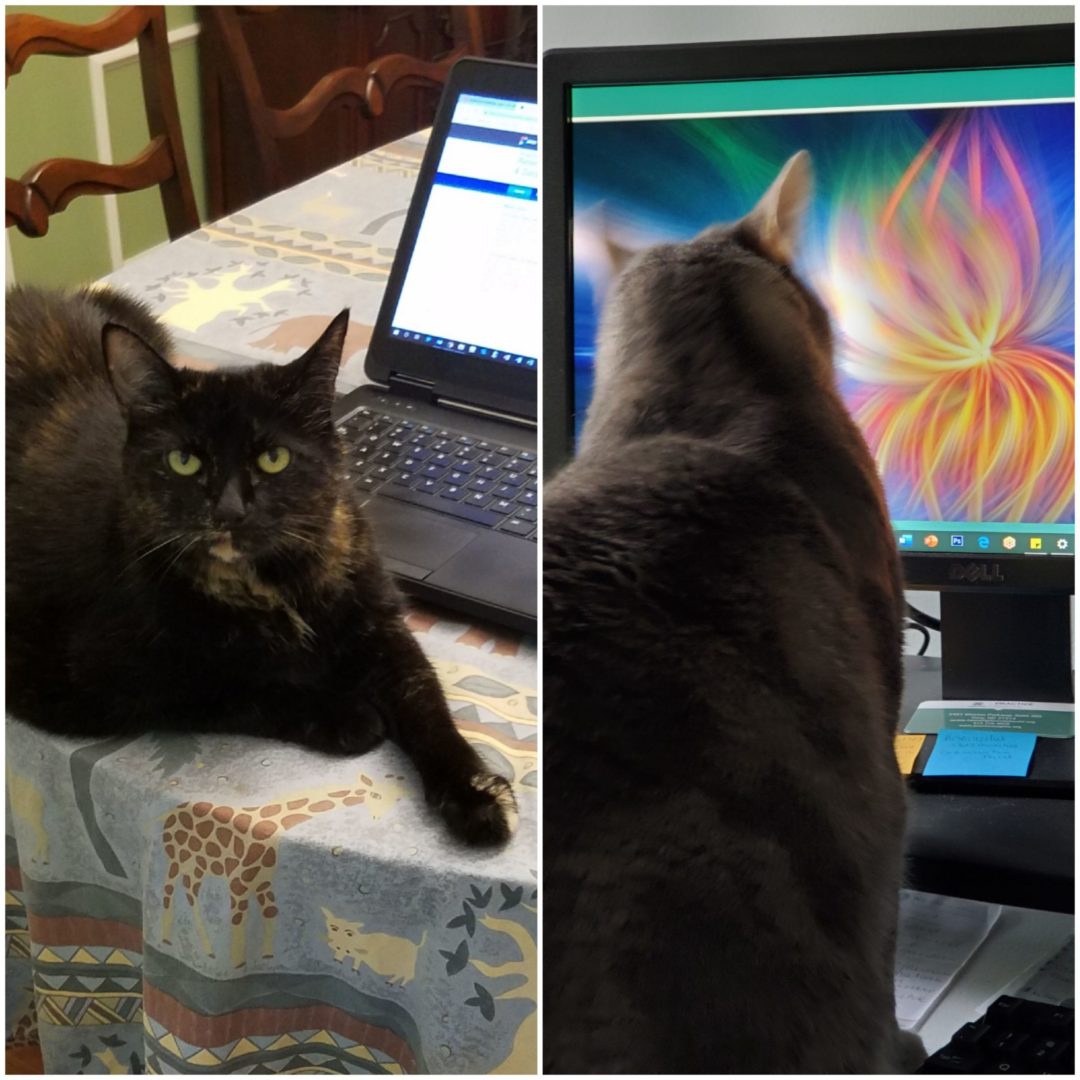
Edie (left) doesn’t take “no” for an answer. She will grind her office’s work to a halt and refuse to move until she gets her pets. Pearl (right) is the more intellectual of the two. You can often find her searching for deeper meaning in her computer’s screen saver.
Freya Jane, M.E.O.W., Center of Excellence for Integrated Care
Freya Jane, M.E.O.W., supervises and reviews all of her human’s reports before they can be submitted. She is the boss of her virtual office, and she is known for ruling with an iron fist.
Frida Pawlo, Rural Forward NC

Frida Pawlo has finally accepted that her coworker is not leaving the house any time soon—on the condition that she gets the bed during daytime hours.
Ila and Abbey, North Carolina Oral Health Collaborative

Ila and Abbey enjoy sleeping on the job most of the day. They have been referred to HR to work on their productivity, as well as their video chat etiquette.
Lydia, Center of Excellence for Integrated Care

Lydia is busy adapting to her new shared workspace—humans can be so disruptive when they’re home all day—so she sent in a picture from her younger years.
Peanut, Rural Forward NC

Peanut is busy adapting to her new work environment. She misses getting out in the community and meeting her partners where they are.
Since moving to remote work, Peanut has been caught sleeping on the job a few times. We understand how tempting the sun can be, but we’ve had to refer her to HR to develop a pupformance improvement plan.
Pepper and Marley, Center of Excellence for Integrated Care

Pepper and Marley have finally grown to accept that there will be no dog park adventures in the future, but they find consolation in the fact that their owners are home. All. The. Time. They sleep on the job, yell during calls and video meetings, and have a bizarre fascination with all squirrels and birds that quite frankly is becoming a little entertaining to the rest of us. TBD on how their performance evaluations will be next month…
Phoebe, Rural Forward NC

Phoebe, aka Feebs, Feebo, or Sneako, works at the Graham-based FHLI satellite office. Phoebe has quickly demonstrated her effectiveness as a footwarmer, and she has a knack for team-based work, playing a critical role in her office’s fetch and lap-sitting duties.
Phoebe’s performance in the last month has been spectacular, and her supervisor has recommended her for a promotion.
Sheldon Lee Schribman, B.S., M.S., M.A., Ph.D., Sc.D., FHLI Communications

Dr. Sheldon Lee Schribman, B.S., M.S., M.A., Ph. D., Sc. D, is by far the best educated member of the FHLI team. He has been social distancing since before it was cool. Dr. Schribman does not appreciate being around anyone other than his mom, so this remote work situation is really working out well for him. He spends his days eating his weight in treats and “greeting” the UPS guy at the front window.
Now, if only those pesky drapes would get out of his way…
NCOHC is a program of the Foundation for Health Leadership & Innovation. For more information and to stay up to date, subscribe to the NCOHC newsletter. If you are interested in becoming an NCOHC member, you can also fill out our membership form. It’s free!