Let’s take a moment to review an all-too-familiar scenario for many North Carolinians.
Martha lives in rural Tyrrell County, North Carolina, where there are no practicing dentists. She works a full-time job while raising her two children. So, she decides against making the hours-long round trip to the nearest dental office one county over to receive a cleaning and checkup.
Let’s face it: for Martha, the cost of transportation, the dental service itself, and the pay lost while she is away from work make for a steep price for care. On top of that, she knows that she may have to schedule a follow-up visit—and take time off from work again, find someone to pick up her children from school again, pay for gas again—if she has any cavities that need filling.
So Martha waits.
Sadly, what started as a bit of sensitivity develops into an unbearable toothache, which lands her in the emergency department (ED). In the ED, she is prescribed an opiate to deal with the pain and an antibiotic for the infection, and she is told to “follow up with your dentist.”
In a month or so, however, Martha, like so many others, ends up right back in the ED when her infection, which has never been directly treated, flares up again
Martha isn’t alone in this situation.
This story is reality for hundreds of thousands of North Carolinians who, for various reasons, cannot access oral health care.
A Better Way: The Promise of Teledentistry
Teledentistry is a promising innovative tool that could play a critical role in increasing access, especially in rural areas like Tyrrell County.
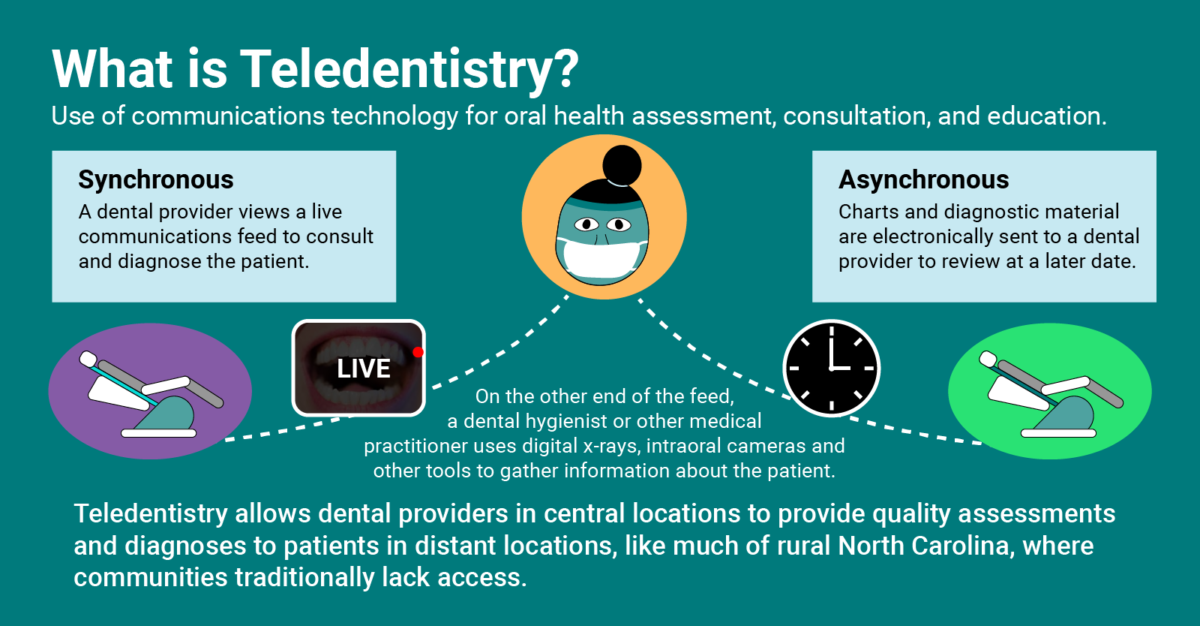
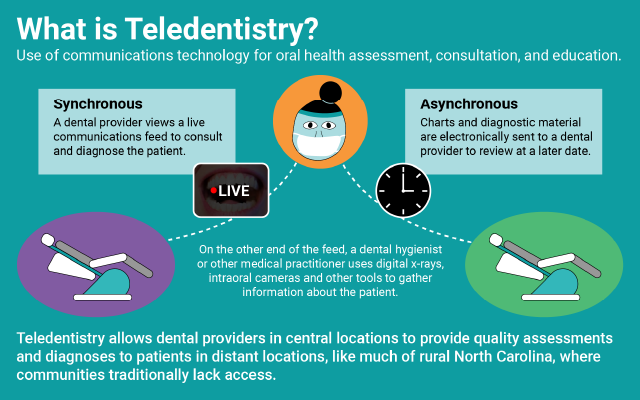
What is Teledentistry?
The use of telecommunications for dental exams and assessments, consultations between dental providers, and direct education for patients, among other uses. Teledentistry is a treatment tool that has incredible potential for increasing access to quality dental care in communities that traditionally lack access, especially in rural areas without practicing dentists.
Imagine this:
The next time Martha winds up in the hospital for her toothache, she is connected with a dentist in Chapel Hill via a live video feed. A medical professional takes digital x-rays of Marhta’s mouth and uses an intraoral camera to allow the remote dentist to take a look at her teeth. The dentist quickly diagnoses her abscessed tooth, prescribes Martha the correct antibiotic to help fight the infection, and helps her schedule an appointment for treatment.
With her oral health issue resolved, Martha finally breaks the cycle of hospital visits that she would have otherwise endured.
While Martha had never seen a dentist up until this point, she has always kept up a good habit of visiting her local federally qualified health clinic for an annual checkup. The next time she visits, she learns that the clinic now offers asynchronous teledental services in partnership with East Carolina University.
Synchronous and Asynchronous Teledentistry
Synchronous is a fancy word that means “at the same time.” In synchronous teledentistry, a dentist is connected via a live video feed to review material, assess the patient in real time, and provide direct patient counsel, if needed.
Dentists who practice asynchronous teledentistry are sent diagnostic information such as digital x-rays and pictures from intraoral cameras to review at a later date, giving them time to look at all the material and put together a comprehensive treatment plan based on the patient’s unique needs.
Digital x-rays and pictures from an intraoral camera are sent to a dentist who works through East Carolina University. She reviews Martha’s records later that week. Fortunately, this time there is no need for further treatment, but the dental provider does advise that Marhta floss more regularly.
Martha’s children have also never seen a dentist. Luckily for them, a dental clinic was recently established at their school and a dental hygienist provides them the same asynchronous teledental services that their mother received at the medical clinic.
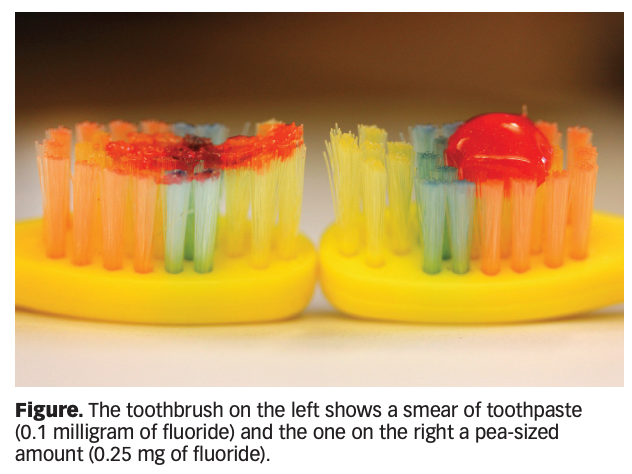
The hygienist provides Martha’s children with fluoride treatments, dental sealants, and a thorough cleaning. The dentist who reviews their digital x-rays and other diagnostic information determines that they have no cavities, but that they both do have moderate gingivitis. The hygienist learns that the two have had to share a toothbrush, so the clinic provides them with two new toothbrushes and tubes of fluoride toothpaste.
From in-school clinics to emergency departments, teledentistry is a promising asset that could significantly improve access and equity in oral health care across North Carolina. For families like Martha’s, simple diagnostic services completed through teledentistry could drastically increase tangible access points to dental services, and in return prevent significant oral health burdens downstream.
The Tools of Teledentistry
Teledentistry can seem daunting, especially when it comes to modernizing an office to meet the technological needs of remote care. Unlike many variations of telehealth, however, the tools of teledentistry are actually quite simple. The basic necessities are:
-
A digital x-ray system
-
An intraoral camera
-
Electronic patient records
Most dental practices already use digital x-rays and intraoral cameras, and practices across the country are rapidly making the switch to electronic record-keeping. Compared to other telehealth services, the startup cost for teledentistry is relatively low.
By helping break the cycle of emergency department visits for oral health crises, medical costs for patients and the healthcare system as a whole could be significantly reduced. This is especially important in our rural communities. Cutting the uncompensated care costs burdening rural hospitals across the state could go a long way in attaining financial solvency. Additionally, inserting a dental professional into the hospital setting via teledental services could be an important way to combat the opioid crisis, reducing the number of unnecessary opiate prescriptions often given to patients with oral health emergencies.
Want to Know More?
NCOHC is taking a trip later this week to tour the state-of-the-art Center of Excellence for Telehealth at the Medical University of South Carolina. Stay tuned for our report from the trip!
Also, join us on June 3, 2020, for Oral Health Day! Oral Health Day is NCOHC’s annual advocacy event at the North Carolina General Assembly. This year we will focus our discussion on pathways to successful teledentistry in our state. Click here for more information and to register today!

Sign up for NCOHC’s newsletter list to receive updates on stories like this one directly to your inbox.
NCOHC is a program of the Foundation for Health Leadership & Innovation. For more information and to stay up to date, subscribe to the NCOHC newsletter. If you are interested in becoming an NCOHC member, you can also fill out our membership form. It’s free!