COVID-19 has impacted virtually every aspect of human life for the past two years. From retaining steady employment and income to maintaining preventive medical care, healthy habits, and more, things got a bit more difficult for most everyone, and a whole lot harder for many.

COVID-Oral Health Connection
Earlier in the pandemic, we published an initial overview of the ways that the virus has impacted oral health. As we enter 2022, with a hopeful light at the end of the tunnel, we are taking another look at the connection between COVID-19 and oral health to break down the many ways the pandemic impacts our mouths.
Here’s a brief review of what we know so far.
Loss of Taste and Smell
From the beginning of the pandemic, loss of taste and smell have been prominent symptoms of COVID-19. As the first recognized oral manifestation of the virus, loss of taste was an early indicator of infection, even as testing and other precautionary measures were still ramping up.
Loss of taste and smell, which are typically grouped together in part due to the similar nature of the two senses, continue to be significant issues for many diagnosed with COVID-19. They are also often among the longer-lasting impacts of the disease. Like many COVID-19 symptoms, however, people who have contracted the virus have a wide range of experiences with the loss of these senses.
In some cases, loss of taste and smell lasts a short period of time before returning to normal, and many who contract COVID-19 don’t lose these senses at all. But in others, sensory loss lasts months, and there are even some cases where the loss of taste and smell seems to be permanent.
Treatment for COVID-related Loss of Taste and Smell
“There are frustratingly few interventions” to treat taste and smell loss, according to a Journal of the American Medical Association (JAMA) commentary. One of the only successful options is olfactory (smell) training. This treatment basically involves regularly smelling a variety of scents. While the mechanisms that make this remedy work are still largely unknown, it has demonstrated a significant level of success.
Physicians and researchers at Thomas Jefferson University Hospital are currently developing another potential treatment: topical platelet-rich plasma (PRP). PRP, which is commonly used for injuries like tennis elbow and muscle pulls, has shown promising results in early trials for treatment of loss of taste and smell.
Dry Mouth and Oral Lesions
While loss of taste and smell were among the first widely known symptoms of the virus, dry mouth has become the most common oral manifestation of COVID-19, present in 43 percent of cases.
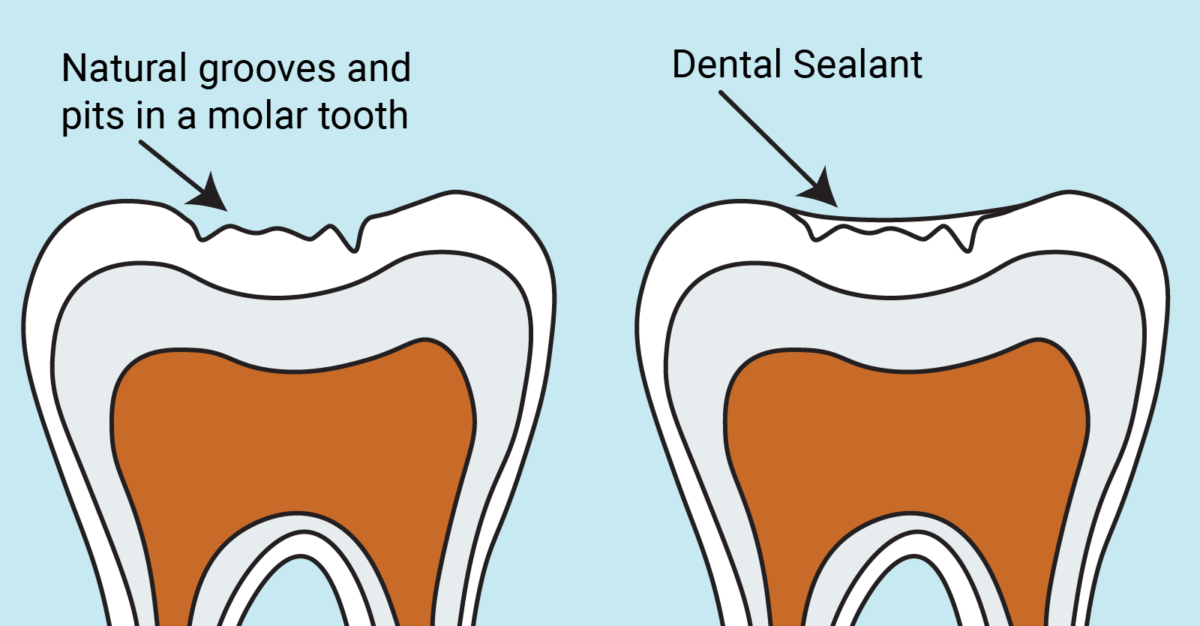
Dry mouth has the potential to lead to or intensify existing oral disease. Saliva is an oral health powerhouse — it helps defend against decay-causing acids and bacteria. With less saliva, people who contract COVID-19 and experience dry mouth are at greater risk of tooth decay and gum disease.
Researchers have also found a significant correlation between COVID-19 infection and oral lesions. Again, the exact mechanisms connecting the virus and the oral manifestation are not clear, and there is a wide variety of types of lesions that have been documented. Ranging from canker sores to herpes-like sores, oral thrush, and more, these lesions were found in 20.5 percent of patients in a study surveying 2,491 cases of COVID-19.
Treatment for Dry Mouth and Oral Lesions Due to COVID-19
According to the Mayo Clinic, dry mouth treatment options include:
- Stay hydrated
- Reduce caffeine intake
- Don’t use alcohol-based mouthwashes
- Stop using tobacco
- Use a humidifier at night
- Use an over-the-counter dry mouth mouthwash
Oral lesion symptoms associated with COVID-19 vary widely. Minor canker sores generally clear up on their own with no treatment, and there are a variety of mouth rinses and topical products available for more persistent sores. For other symptoms like oral thrush, antifungal medicines may be necessary. Because of the wide variation in lesions, the best approach if you are experiencing these symptoms is to consult your dentist.
Understanding COVID-19 and Its Oral Manifestations
To say the least, COVID-19 is an incredibly confusing virus. The list of potential effects is seemingly endless and disconnected, ranging from flu-like symptoms like fever, cough, and sore throat to:
- Shortness of breath, and difficulty breathing
- Headaches
- Loss of taste and/or smell
- Oral lesions
- Brain fog
- Pink eye, light sensitivity, and sore or itchy eyes
- Rashes
- Swollen or discolored extremities
- And more
Some of the most prominent symptoms are very similar to the flu, suggesting that COVID-19 is a respiratory disease. But researchers are continuing to find evidence indicating that COVID-19 might be a vascular virus – a disease of the blood vessels.
Looking at COVID-19 as a blood disease can help demystify the variety of seemingly disconnected symptoms. In the dental community, we are familiar with the important role of blood vessels in the mouth-body connection. With COVID-19, blood vessels could be the link between stroke-like brain impacts, respiratory problems, and oral manifestations.
COVID-19 and Oral Health Equity
Beyond direct connections between COVID-19 and the mouth and the nearly endless list of symptoms associated with the virus, there is another long list of impacts that make their way back to our mouths. Nearly every social determinant of health has been exacerbated during the COVID-19 pandemic, and they all have oral health repercussions.
Prior to the pandemic, the U.S. poverty rate was at its lowest point since 1959. Despite supplemental programs to offset income loss early in the pandemic, poverty rates for adults and children alike have increased. Many people struggled (and continue to struggle) to get enough food, retain steady employment, and maintain stable housing — all of which have known links to oral health and overall health.
The bottom line: Outside of the dental office, it has been much harder for millions of people to maintain good oral health habits during the pandemic.
Inside the dental office, things also became harder when the pandemic hit.
- There is a plethora of anecdotal evidence from dentists across the country who have seen more patients with stress-induced cracked teeth.
- Fear of seeking care due to possible COVID-19 exposure continues today, putting people at risk of more extensive treatment needs down the road.
- The widening income gap and shaky employment situations have left many without the insurance necessary to maintain regular preventive appointments.
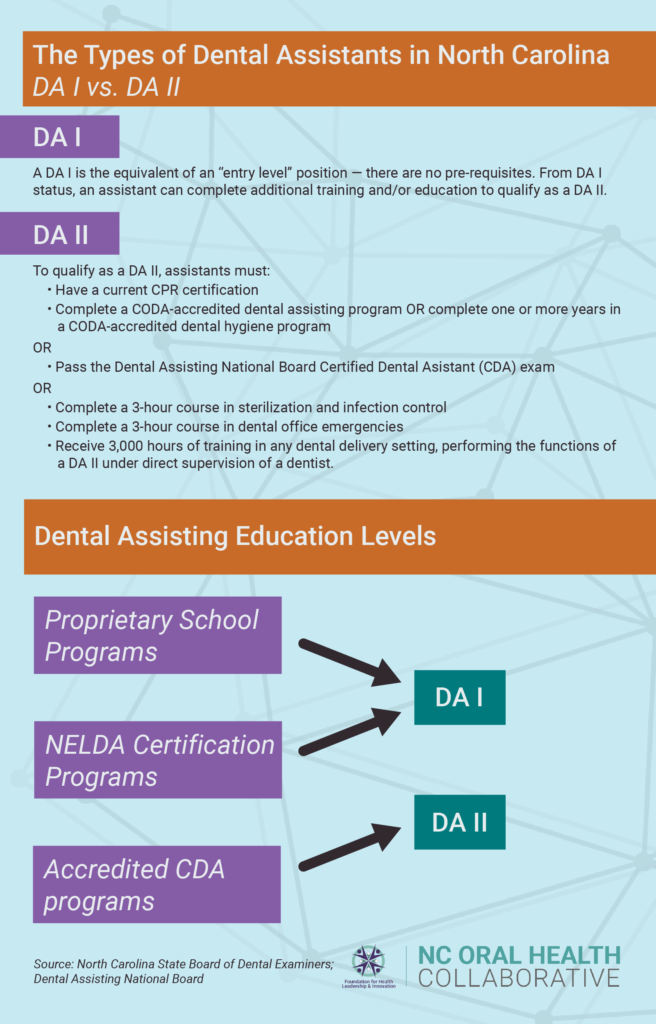
- Dental staffing shortages, a problem before COVID-19, have become more severe during the pandemic, especially among hygienists and assistants.
Oral Health & COVID-19: Where Do We Go from Here?
The list of connections between COVID-19 and oral health could go on and on. For example, dental researcher Faleh Tamimi is leading a study of similarities between COVID-19 and periodontal disease co-morbidities, finding that people with COVID-19 and gum disease are 3.5 times as likely to be admitted to an ICU and 4.5 times as likely to be put on a ventilator. In the months and years ahead, we’ll continue to keep a close eye on this and other research exploring the link between COVID-19 and oral health.
At the end of the day, however, one thing is clear: the many ways COVID-19 impacts oral health continue to be significant.
The pandemic could, and should, be an opportunity as well. With so many in need, and with so much focus on health care, we have an incredible opportunity to look at structural changes to dramatically increase access to care.
NCOHC and our incredible coalition of partner organizations and advocates are taking strides to map out the future of oral health care – a. future that includes everyone, everywhere. Learn more about current initiatives and ways you can get involved today at oralhealthnc.org/nc4change.
NCOHC, a program of the Foundation for Health Leadership & Innovation, works to advance systems-level changes, improving the overall health and well-being of all North Carolinians by increasing access and equity in care. To stay up-to-date and get involved, join us today as a North Carolinian for Change.