Visiting the dentist can be anxiety-inducing, leading people to avoid seeking care. The common fear of the unknown, financial concerns, and past negative experiences can intensify these worries. Luckily, there are many ways to address dental anxieties and help improve access to oral health care.
Trust and Communication
Whether stories come from family and friends or social media, adverse experiences at the dentist are easy to find. This reality is important for providers to understand. There will be patients who come to an appointment afraid of what may happen. There will also be people who never seek out care due to dental anxiety, fear, and shame about the condition of their oral health.
A provider who actively builds patient relationships can create a more comfortable environment that puts people at ease. Through genuine, trusting relationships, dentists can better understand patient concerns, answer questions with kindness and compassion, and clearly explain dental terminology. This dialogue and information exchange can help people weigh the pros and cons of proposed treatments.
Individuals who trust their dentist will also feel more comfortable sharing personal information without fear of judgment. These additional details can give the provider a better idea of which treatments to recommend and identify any potential obstacles. Establishing a relationship will increase the patient’s willingness to seek help from their provider to improve any conditions that may develop and keep existing ones in check.
Understanding Treatments
Quality patient-centered care is paramount. Not everyone knows why fluoride is beneficial, why teeth become sensitive, how a cavity gets filled, or the root canal process. However, understanding these procedures can help people feel safe when receiving care.
Dentists, hygienists, and assistants can often explain these treatments. Clear explanations can help patients build trust with the entire dental team by ensuring they have a positive experience throughout the ongoing process of receiving care.
When thinking of ways to develop positive relationships with patients, providers should consider the following:
- Make sure to thoroughly explain procedures before the appointment day, if possible.
- Allow adequate time for patients to ask any follow-up questions.
- Offer guidance on at-home hygiene practices and product recommendations.
- Discuss key ingredients to look for in toothpaste and mouthwash to equip patients with the information they need to look for the best products.
- Learn about, seek training in, and incorporate trauma-informed care and motivational interviewing practices.
Over time, as treated conditions improve, patients will feel more confident in their provider, encouraging them to follow any routine adjustments they recommend.
A trusting, collaborative patient-provider relationship is essential for positive outcomes. The role of a health care provider is to educate patients while providing high-quality care aimed at improving overall quality of life in the short- and long-term.
NCOHC, a Foundation for Health Leadership & Innovation program, works to advance systems-level changes, improving the overall health and well-being of all North Carolinians by increasing access and equity in care. Sign up for our monthly newsletter to join the network and get involved!
Related Content & Resources
- Dental Anxiety and The Role of Providers in Facilitating Approachable Care
- Oral Health Care Integration Case Study Part I: Social Work in Dentistry
- Oral Health Care Integration Case Study Part 2: Social Work in Dentistry
- NCIOM Task Force: 14 Recommendations for Patient-Centered Oral Health
- Trauma-Informed Care in Oral Health Care: The role of dental hygienists
- Using Motivational Interviewing in Dentistry Video Series
How to Become a Dental Assistant
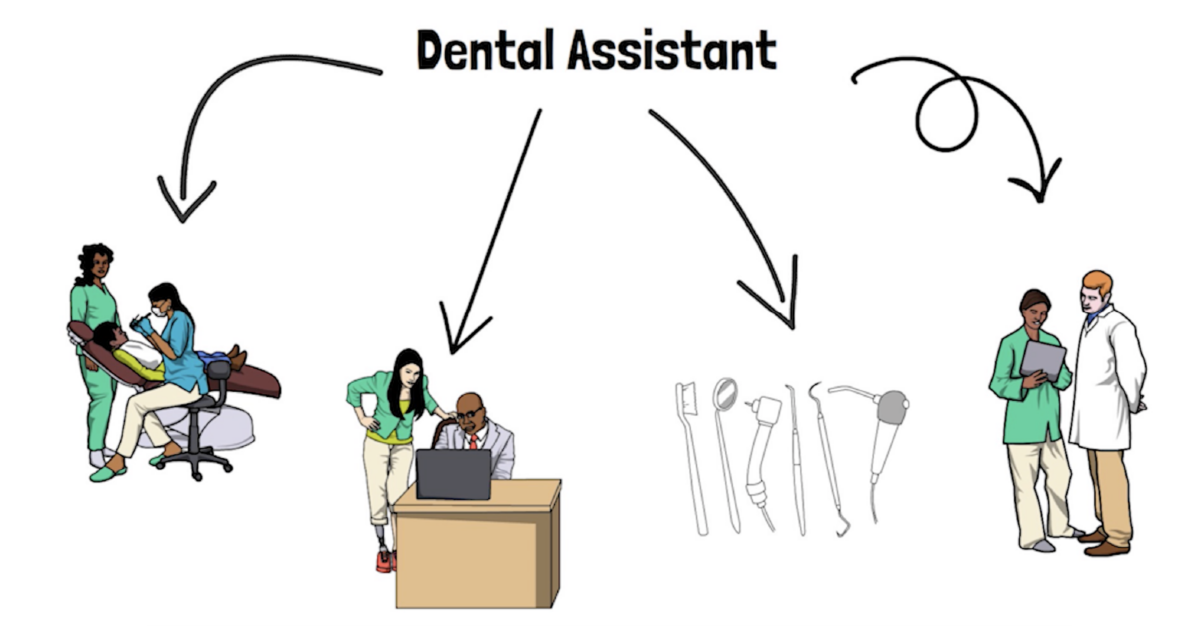
Dentists, dental assistants, and dental hygienists work together as a team, making sure a dental office functions like a well-oiled machine. Have you ever considered a career as a dental assistant? If you have, NCOHC has some tips for you!
As a dental assistant, you can fill plenty of different roles. Some work chairside, helping dentists and hygienists care for patients. You can also work as:
- An office manager, helping schedule appointments, handling day-to-day activities, and managing the business side of dentistry.
- A sterilization technician, keeping dental instruments and treatment rooms clean and ready to use.
- A treatment plan coordinator, working with providers and patients to map out health care needs and keep track of appointments and follow-up care
- And more!
Becoming a Dental Assistant
There are several paths you can take to become a dental assistant. If you enroll in a program at an accredited school, you can graduate and enter the workforce as a DAII (Dental Assistant II).
Proprietary school programs also provide a condensed form of dental assistant training. You graduate ready to enter the workforce as a DAI (Dental Assistant I) through these programs or programs offering National Entry Level Dental Assisting (NELDA) certification.
Alternatively, dental assistants can jump in and train chairside, taught by a dentist in a dental office.
What’s the difference?
A DAI is an entry-level assistant. While the training is quicker for DAIs, DAIIs earn higher salaries and have more options for the roles they can fill in a dental office.
If you want to learn more, check out our interview with Kati Garrett, a dental assistant and educator overseeing Catawba Valley Community College’s dental assisting program.
This blog post was originally written by NCOHC intern Sydney Patterson and later edited by Allison Hackman

“It’s uncomfortable to think of a social worker in your space, and it’s uncomfortable to think about asking patients the questions that we ask. So, if it feels uncomfortable, lean into it because there’s going to be something good that comes from it.”
The University of North Carolina (UNC) Chapel Hill School of Social Work and Adams School of Dentistry (ASOD) partnered to provide dental and social work students with interprofessional workforce development and learning opportunities related to social drivers of health (SDOH). Integrating dental and social work education provides students from both cohorts with valuable experiences they will carry into their future practices.
Jamie Burgess-Flowers, MSW, LCSW, Kelsey Yokovich, MSW, and Lisa de Saxe Zerden, MSW, PhD published a research paper titled “The social determinants of health, social work, and dental patients: a case study” to document the first-year implementation of this model at the dental school. If you haven’t already, read part one of this case study for more background information to join us in the conversation with Burgess-Flowers and Yokovich from the beginning.
In this blog post, Burgess-Flowers and Yokovich share insights into the value of social work integration in dental care, the need for buy-in to promote sustainable systems-level changes, and the importance of continual learning.
Case: Social Work Consultation at a Dental Clinic
Burgess-Flowers told a story about one of her first days working in a dental clinic that demonstrates how integrating dental education and social work can transform patient and provider experiences for the better. A dental student approached her seeking guidance after completing a young adult patient’s health history intake. He noticed significant decay throughout their whole mouth, “I’m really concerned because this patient in their health history interview said that they don’t do any drugs.”
Although that patient had a level of decay often seen in patients with methamphetamine substance use disorder, Burgess-Flowers consulted with the student. She encouraged him to continue asking questions rather than jumping to conclusions. As it turned out, the patient worked extended Emergency Medical Services (EMS) shifts, drank Mountain Dew for the caffeine and hydration without water, and had little to no time for personal oral hygiene.
Though a patient may be struggling with a substance use disorder, this dental student learned to challenge his assumptions and remain open to other possibilities. Social drivers of health (SDOH) come in many forms, including employment type, dietary choices, and more, as this patient experienced.
The student will carry what he learned from this firsthand work experience long after graduating from dental school. “Having [this] foundational educational piece is going to be important for shaping a generation of providers that really think about the care of an individual as whole rather than siloed,” said Yokovich.
Buy-in: Driving Sustainable Change
Social work and oral health integration remains a fairly new concept that Yokovich and Burgess-Flowers hope will expand in the future. They discussed the importance and challenges of getting buy-in from students, educators, university leaders, providers, policymakers, and anyone else involved in the care system.
Burgess-Flowers spoke about the challenge of getting buy-in from some folks in dental education who have yet to see value in integrating social work into the curriculum. “When I started at UNC, one of the faculty members who was an oral medicine specialist looked at me, and he said, ‘You need to understand that what you’re doing is incredibly valuable. You are also asking a group of folks who have been trained to use a two-millimeter point of view to look at a tiny piece of disease on the surface of a tiny tooth to back up to a two-thousand-foot view of a patient,” she said.
Yokovich, the final and only macro (aka community management policy practice) social work student to participate in the UNC School of Social Work and ASOD program, said, “There was a lot of push-back, especially when I was talking about racism and the influence that has over practice.” Building on that, Burgess-Flowers said, “Now, social work is more synonymous with social justice, and people think that we’re going to be bringing up the uncomfortable things.” She told us it takes time to overcome “people’s perceptions of what a social worker is and what we bring to the table.”
When it comes to integrating social work and dental education, Burgess-Flowers said, “Buy-in is a really slow process for me, but it’s also all about that end goal that requires a lot of patience to get there.” Her vision is that as social work becomes embedded into dental education and dental practices, the holistic approach will trickle down until new employees, faculty, and students “say, well, this is just the way we do things.”
Key Takeaways: Lean in & Keep Learning
In their closing statements, Yokovich and Burgess-Flowers encouraged anyone in health care and education to stay open to continual learning. “An overarching message is for providers and folks who are in the educational space to keep an open mind when they feel uncomfortable. Usually, good things come out of that,” said Yokovich.
“It’s uncomfortable to think of a social worker in your space, and it’s uncomfortable to think about asking patients the questions that we ask,” said Burgess-Flowers. “So, if it feels uncomfortable, lean into it because there’s going to be something good that comes from it.”
They both hope to see this interdisciplinary work continue and care integration implemented across all areas of health care.
NCOHC, a Foundation for Health Leadership & Innovation program, works to advance systems-level changes, improving the overall health and well-being of all North Carolinians by increasing access and equity in care. Sign up for our monthly newsletter to join the network and get involved!
Related NCOHC Blog Posts
- Oral Health Care Integration Case Study Part I: Social Work in Dentistry
- Diversity in the Workforce: An Opportunity for Change
- Racism, Food, and Your Mouth: Parallels Between Food and Oral Health Equity
- How the World Around Us Impacts Our Oral Health: An Intro to the Social Determinants of Health
- Social Determinants of Health: How the World Around Us Impacts our Mouths
- Social Determinants of Health – Structural and Governmental Influences
Oral Health Day 2024 Recap
Thank you to all who joined us for Oral Health Day 2024! We’re excited to share that we had our highest participation yet. This year, NCOHC presented two new awards and we heard from expert speakers, including a “North Carolina’s Oral Health Workforce, by the Numbers” presentation and panel discussion.
If you couldn’t make it, you can watch the full recording. Below, you will also find details about our awardees, NC oral health workforce data, panel discussion highlights, and resources from our speakers.
Oral Health Advocate Awardees
NCOHC staff presented two awards during this year’s event. Dr. Katrina Mattison-Chalwe received the Oral Health Community Award, and Dr. Frank Courts received the Oral Health Champion Award.
Dr. Katrina Mattison-Chalwe: Oral Health Community Awardee
In addition to her full-time job leading a public health dental team and a mobile dental unit, Dr. Mattison-Chalwe also finds time to lead a nonprofit called Smiles for Jesus. She was instrumental in co-chairing the recent North Carolina Institute of Medicine Oral Health Transformation Task Force and has proven herself to be an important voice in the work to improve access and equity in care in North Carolina.
Dr. Frank Courts: Oral Health Champion Award
Dr. Courts was the first dentist in North Carolina to pilot a school-based oral health program. He is a frequent participant in task forces aimed at improving care, and he is an accomplished mentor of oral health professionals, encouraging the workforce to center patients in the care they provide.

“North Carolina’s Oral Health Workforce, by the Numbers”

Connor Sullivan, PhD, presented data from the Cecil G. Sheps Center for Health Services Research at UNC, which informs state, regional, and national workforce policy. Independent of government and health care professionals, the NC Health Professions Data System (HPDS) has 43 years of continuous, complete licensure (not survey) data on 21 health professions from 11 boards. The system is a collaboration between the Sheps Center, NC Area Health Education Centers (NC AHEC), and the health professions licensing boards.
During his presentation, Dr. Sullivan broke down the statewide movement of dentists, the concentration of dentists by county, the concentration of dentists by county per dental school, the top five dental schools in the NC workforce, race/ethnicity of dentists and registered dental hygienists (RDH) versus population diversity, and the number of active RDHs over time (2000 to present). A few highlights include:
- 5.5% net gain in number of NC dentists after imports and exports
- 60% of newly graduated dentists went to just 5 out of 100 counties in NC
- Eastern Carolina University (ECU) graduates are nearly two times more likely than all other NC programs to serve rural areas
One of the big takeaways from his talk was that the number of dentists in North Carolina is improving, but distribution and diversity remain challenges.
Oral Health Workforce Panel Discussion

This year, Hugh Tilson, JD, MPH, moderated the Oral Health Workforce panel discussion and asked about NC’s dental workforce challenges and opportunities.
Dr. Courts highlighted the importance of community-based recruitment and introducing young people to oral health opportunities when considering their career options. He reported that the NC Dental Society (NCDS) awarded 16 dental assisting scholarships and 20 stipends for dental assistants to take the certification exam. He also shared that:
- A new high school program focused on introducing students to the dental field is coming soon.
- There are two new dental assisting programs at Alamance and Southwestern community colleges.
- There are two new dental hygiene programs at Isothermal and Southwestern community colleges.
Andy MacCracken, MPA, discussed the need for critical health workforce coordination, longer-term workforce development, and community-based, non-licensed, non-certified oral health team members.
Stephanie McGarrah, MPP, shared about the $110B that NC received from across six bills in 2020, which is still being directed toward dental practices, businesses, and health systems. She also highlighted the growing trends in high schools to encourage students to explore career opportunities that do not require a four-year college degree.
Melissa Smith, MSEd, RT-R, CT (ARRT), CNMT, spoke about NC’s 13 hygiene programs and 19 CODA-accredited DAII programs. She also shared that the General Assembly provided funds to start and expand health care programs statewide. So far, $4M has gone to expanding dental assisting programs at two schools, starting dental assisting programs at five schools, and starting dental hygiene programs at two schools, including one evening program.
What Keeps You up at Night?
For Smith, the need for qualified faculty, the funding to pay them adequately, and clinical space are top priorities.
McGarrah said recruitment for oral health professionals remains a crucial piece of addressing the ongoing workforce challenges.
MacCracken emphasized the need for supporting and increasing the number of non-licensed, non-certified oral health team members who are also part of the communities they serve.
Dr. Courts thinks it is vital to build and maintain strong community relationships, focus on recruitment in the community, and prioritize introducing young adults to the oral health field.
How Can Oral Health Professionals Engage in NC Workforce Initiatives?
McGarrah shared a new tool from the Department of Commerce called Reality Check. It enables folks to build a budget for things they want and then matches them with jobs that can provide a salary that supports their budget and details about the education required. She emphasized that there is a shifting focus in high schools for students to consider future careers that do not require four-year college degrees.
Smith said it is important to start the workforce pathway as young as elementary school by introducing students to opportunities within oral health.
Tilson shared that the NC Dental Society (NCDS) does outreach at high schools and needs volunteers to speak with students. He also mentioned the importance of more public health hygienists with the potential to embed them into the school systems.
Dr. Courts supported the idea of embedding dental hygienists in schools, like school nurses, to increase access to care for children and teenagers.
Stay Connected & Engaged to Oral Health Workforce Development Initiatives in NC
Thank you again to everyone who made Oral Health Day 2024 a success! As our expert speakers discussed, we must invest the necessary time, energy, and resources into oral health workforce development and increasing access to care for communities across our state.
To stay informed about our ongoing programs and initiatives, including those related to workforce development in NC, we invite you to sign up for our monthly newsletter. Stay connected, stay informed, and continue to be a part of our mission to improve oral health for all North Carolinians. We are grateful for your ongoing advocacy and partnership!
Resources from Our Speakers
- NC dentist US vs NC 2001-2022 (American Dental Association (ADA)-member exclusive content)
- ADA Health Policy Institute (includes NC’s rank compared to other states, as well as import and export data)
- UNC Sheps Center
- UNC Program on Health Workforce Research and Policy
- NC DHHS Health Professional Shortage Area (HPSA) 2023 data
- KFF Dental Care Health Professional Shortage Areas (HPSAs)
- NC Dental Society work opportunities
- NC Department of Commerce Reality Check tool
“I love our pediatrician, but I pray that he doesn’t leave our area because there are so many providers leaving,” said Rachel, a mother of two who lives in Wayne County, North Carolina. “It’s going to be hard for our family if he does.”
“For me personally, if my son were sick, I would not be able to get an appointment today. I would have to wait for an emergency appointment or take him to the emergency room,”
said Rachel. “We just have a lack of providers here, and we’re losing providers. They’re leaving our state to get paid better elsewhere, to get treated better elsewhere.”
Rachel’s sons have had Medicaid insurance for their entire lives, but Rachel herself went uninsured until recently. She qualified for Medicaid in 2020 after a severe case of COVID-19 that left her with long-COVID symptoms.
Gaining access to Medicaid insurance has allowed Rachel to focus on her own health, which she had to deprioritize partly due to the cost of accessing care without insurance.
“I wasn’t able to work much of the year as a result,” said Rachel. “So, I got Medicaid, and I didn’t lose it when I went back to work because of the pandemic supports. And I would have lost it if North Carolina hadn’t expanded Medicaid last year.”
Gaining access to Medicaid insurance has allowed Rachel to focus on her own health, which she had to deprioritize partly due to the cost of accessing care without insurance.
“I’ve transformed these past three years because I’ve finally been able to care for myself,” she said.
Rachel grew up with a single mother. Family financial constraints made dental care and primary care luxuries throughout her childhood. To get to where she is today, Rachel faced a long journey navigating a health care system often ill-equipped and, at times, seemingly hostile to her needs.
“I had to be very sick to see a doctor or dentist,” she said. “Even though I wasn’t seeing a dentist, I was very good about brushing. I wasn’t flossing like I should, but I was brushing. And what got me into it was preschool. They were all about dental care. They gave us visuals, and we brushed our teeth at school.”
In her early 20s, Rachel decided to see a dentist for the first time. Her wisdom teeth were causing pain and needed to be removed. She had never been to a dentist for a cleaning or any other service, but she had to address the pain she felt.
“The dentist referred me directly to an oral surgeon, and I will never forget how mean he [the oral surgeon] was,” said Rachel. “I think he thought I wanted pain medicine. I didn’t, I wanted to understand why I was in pain. I couldn’t eat, I was losing weight. And that experience scared me. I didn’t want to go back for that next cleaning with a dentist because of what I experienced with the oral surgeon.”
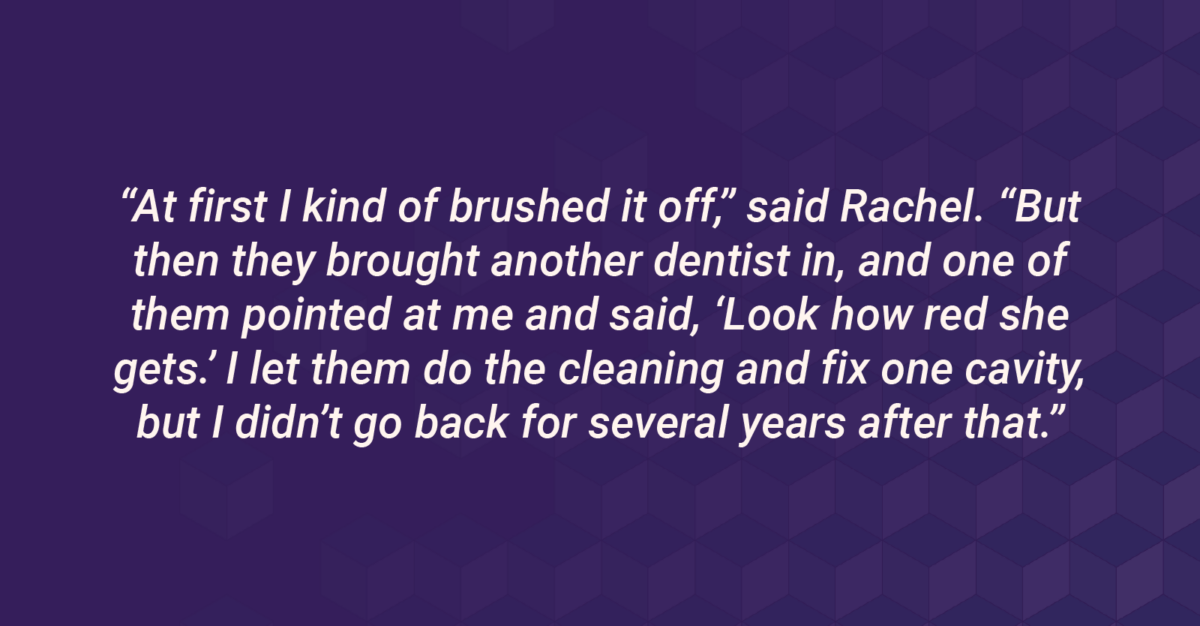
After that, Rachel avoided returning to a general dentist for her first cleaning. When she did make an appointment, her provider laughed at her for being scared in the office.
“At first I kind of brushed it off,” said Rachel. “But then they brought another dentist in, and one of them pointed at me and said, ‘Look how red she gets.’ I let them do the cleaning and fix one cavity, but I didn’t go back for several years after that.”
In 2020, Rachel needed to see a dentist again. She had an infected tooth that needed to be removed. She credits the dentist she saw then with helping her overcome her fear in dental offices.
“I said, ‘Would your staff be willing to talk me through everything? Walk me through it like I’m a toddler because I’m so scared,’” said Rachel. “The lady that he had assist him during the procedure had been through my experience herself. I thank God he did that because I needed someone with that experience to know what I felt.”
Today, Rachel and her entire family continue to see that same dentist. She credits his caring approach with helping her adjust to regular appointments and improve her overall oral health.
“After that experience, I stopped being scared of dentists,” she said. “I’ve been going to the dentist ever since.”

“Our partners in this effort helped us form one of the most unlikely bipartisan, cross-industry coalitions ever assembled in North Carolina–and we succeeded.”
— Care4Carolina Executive Director Abby Emanuelson speaking about Medicaid Expansion in North Carolina
Medicaid Expansion is one of the greatest public health achievements in North Carolina’s history, even though it is far from the end of the road toward truly healthy communities across our state. In honor of this week of recognition, we’re providing you with an update on Medicaid Expansion since it went into effect last December.
In this blog post, you can learn about the impact of Medicaid Expansion to date and considerations for oral health access and equity for newly eligible beneficiaries.
NC Medicaid Expansion
To recap, Medicaid Expansion extended coverage to people ages 19 through 64 years old who previously fell in the health care coverage gap, meaning they earned too much to qualify for Medicaid but too little to access the Affordable Care Act marketplace. Since expansion began on December 1, 2023, nearly 400,000 newly eligible recipients have already enrolled (about 1,000 daily), which is over half of the 600,000 expected to enroll over the next two years.
After launching Medicaid Expansion, NCDHHS, county health departments, and local social services departments have enrolled recipients faster than other states in the past (all states had the option to expand Medicaid beginning in 2014). Community-based organizations and partners have been essential in spreading the word and helping people enroll in the best plan to meet their needs.
NCDHHS Medicaid Data Dashboard
The NC DHHS Medicaid Expansion data dashboard provides monthly updates on how many people have enrolled through Medicaid Expansion, including statistics by health plan, demographics, and county. During a January 2024 interview, NCDHHS Secretary Kody Kinsley reported that Medicaid Expansion had already covered over $4.8 million in claims for dental services.
Highlights from the dashboard reports through March 2024 include:
- New enrollees disproportionately live in rural communities (96,318 enrollees as of March 2024)
- Over half of enrollees are under 40, with most between 19 and 29 years old
- Anson, Edgecombe, Richmond, Robeson, and Swain counties have seen the highest enrollment rates
Oral Health Provider Shortage & Access to Care
While we celebrate the milestone achievement of NC Medicaid Expansion, we have more work to do. While North Carolina offers all Medicaid recipients oral health coverage, it is not currently listed as a benefit on the Medicaid insurance cards. Many people, from newly eligible recipients to health directors, remain confused about what Medicaid covers.
We also need more oral health providers who accept Medicaid to meet the growing demand. The physician shortage, especially in rural communities, affects beneficiaries and frontline workers alike. During our 2023 Oral Health Day event, keynote speaker Kathy Colville, former President and CEO of the North Carolina Institute of Medicine (NCIOM), put it clearly: “We have truly amazing and exceptional people holding up an inadequate system.”
Only 28 percent of dentists in North Carolina accept meaningful volumes of Medicaid patients. Of those who do, many accept just a few recipients and are not currently accepting anyone new. A contributing factor to this low acceptance rate is that Medicaid dental reimbursement rates remain at the same level as they were in 2008.
Long before NC Medicaid Expansion, dentists advocated for higher Medicaid reimbursement rates for oral health, which falls around 34 cents on the dollar today. Many more providers need to accept Medicaid to meet the demand. “They [Medicaid providers] are woefully underfunded,” said NCOHC Vice President Dr. Steve Cline.
Some estimates among oral health care providers suggest that reimbursement rates need to be at least 75 cents on the dollar to build an adequate private provider network to meet the need. Our incredible public health oral health providers do not have the necessary time, capacity, or resources to serve every Medicaid recipient in the state.
Unless our state and federal governments commit to a massive expansion of public health funding, we need private practice dentists to begin accepting new Medicaid patients as soon as possible.
What’s Next?
Alongside an overhaul of NC Medicaid reimbursement rates, as we continue to enroll communities across our state, we need to both incentivize and make it economically viable for oral and health care providers to practice in rural areas. One path forward is expanding loan forgiveness options for dental professionals in rural communities.
We must also continue to advocate for policies and programs to expand the use of teledentistry. To do this, we need a robust rural broadband infrastructure.
Last year, NCOHC partnered with the North Carolina Institute of Medicine, with support from The Duke Endowment, to launch the Oral Health Transformation Task Force. Their full report with recommendations to transform our current oral health system will be released to the public soon. Stay tuned for more information!
Resources
- NC Medicaid Enrollment Reports
- Medicaid Expansion FAQs
- NC Medicaid Expansion Data Dashboard
- Medicaid.nc.gov
- NCDHHS Medicaid Expansion Portal: Information on eligibility, FAQs, how to apply, and sign-up form for news and updates
- Safety Net Dental Clinic Locations

“I don’t just want whole-person care happening in the clinic, I want to see whole-person education as well.”
Research shows that up to 80 percent of a person’s overall health can be attributed to non-medical factors. These social drivers of health (SDOH)* pose intractable barriers for countless North Carolinians when accessing oral health care. Care integration has been shown to increase access and equity in oral health and benefit both patients and providers.
*Although still widely used, recently, there has been a shift in language from ‘social determinants’ to ‘social drivers’ of health. This change acknowledges that a wide range of nonmedical factors can impact a person’s overall health; however, they do not determine what a person’s health outcomes will be, but rather have the potential to drive them.
The University of North Carolina (UNC) Chapel Hill School of Social Work and Adams School of Dentistry (ASOD) partnered to provide dental and social work students with interprofessional workforce development and learning opportunities related to SDOH. Integrating dental and social work education provides students from both cohorts with invaluable experiences that they will carry into their future practices.
Jamie Burgess-Flowers, MSW, LCSW, Kelsey Yokovich, MSW, and Lisa de Saxe Zerden, MSW, PhD published a research paper titled “The social determinants of health, social work, and dental patients: a case study” to document the first-year implementation of this model at the dental school.
UNC Chapel Hill School of Social Work & Adams School of Dentistry
Dr. Zerden created the program, Burgess-Flowers served as the clinical social work faculty member, and Yokovich contributed as the final and only macro (aka community management policy practice) social work student. Burgess-Flowers built the program and established clinical workflows in the dental settings. When Yokovich joined, she helped develop the programmatic integration, conducted research, and attended the dental school’s research day.
Currently, Burgess-Flowers is an Assistant Professor and the Director of Integrated and Applied Behavioral Sciences at High Point University and Yokovich is the Community Voice Program Coordinator at the Foundation for Health Leadership and Innovation (FHLI).
Before leaving for High Point University, Burgess-Flowers wanted to document their work and hopefully contribute to creating more opportunities for social workers to integrate into oral health care spaces. Yokovich had social work experience as well as working in both oral health spaces and wanted to help develop a model for integrating the two fields.
Burgess-Flowers and Yokovich shared their experiences and vision for integrated care in oral health settings. Join us in the conversation…
Why is this topic important to you?
“I came from a primary care setting, and I was working in integrated care with patients. I thought to myself, ‘This is whole-person care,’ but I wasn’t asking patients about their oral health.” said Burgess-Flowers. “As social workers, we talk a lot about how people need to realize that the brain is part of the body. But we’re just as guilty of leaving out the mouth.”
“I worked in a dental office as a treatment coordinator and saw the lack of resources for folks who might not be able to go to different health care offices because they don’t have the time, transportation, resources, or financial means,” said Yokovich. “If you’re going to go into integrated care, it can’t just be physical, it can’t just be behavioral outpatient, it has to be the whole-health picture.”
Can you speak about the influence of SDOH on oral health disparities and the effectiveness of addressing them through social work integration?
“Dental offices are incredibly, historically, traumatizing and can be very over-stimulating for folks with trauma histories,” said Burgess-Flowers. “One thing I’m big on is being able to explain to [oral health providers] how social determinants of health relate back to something like filling a cavity or placing a crown. That is what dentists have been historically trained [to do]. They’re procedure-based, so they really want to know how what you’re talking about or offering to assist with has an impact on what [they] do or why a patient is here.”
“The demographic of oral health providers does not match the demographics of the United States at large. There’s a very stark contrast between those providing care and those receiving care,” said Yokovich. “Something that Jamie and I tried to do while I was at the dental school was educating oral health providers to think about these systemic issues a little bit differently because they’re the ones who are then going to be taking that into practice.”
How did you see care integration help both students and patients?
“It (dental-social work integration) opened so many doors for patients to receive referrals that they might not have been able to receive before,” said Yokovich. “And being able to express concerns about different areas of their lives as well, which is super interconnected and interwoven into their whole health.”
“We’re seeing less turnover, less no-shows,” said Burgess-Flowers. “We see a lot of improvement with dental students and learners, we see their perspective on patients change. We see their burn-out rates improve. We see them feeling like they have a team of people they can lean on and work with inter-professionally and not have to take everything on themselves.”
What ideal changes do you foresee in dentistry and social work?
“I would love to see the model be standard in dental education. I want to see more social workers, and not just clinical social workers, but also your macro social workers, in dental education,” said Burgess-Flowers. “I want dentists and dental hygiene folks in social work education. I don’t just want whole-person care happening in the clinic, I want to see whole-person education as well.”
“I would love to see buy-in from every aspect of oral health care, whether that’s from the dental education perspective or private practice. And I would love to see providers start getting credentialed with Medicaid and accepting patients who they would not have traditionally accepted in their past practice,” said Yokovich. “Having that foundational educational piece is going to be really important for shaping a generation of providers that think about the care of an individual as whole.”
How do you see this research contributing to your work moving forward?
Burgess-Flowers said, “This [role] really is a beautiful blend of being able to teach dental students clinical skills, communication skills, and being trauma-informed, all the way up to self-wellness, preventing burn-out, thinking about our community, the social systems, and racism, and all of the things that come into health care and interfere with patient outcomes being what we want them to be.”
“In a perfect world,” said Yokovich, “I would love to see integrated care across the board, but I think that just starts with us being advocates now where we’re at in order to make small systemic changes happen, so this paper kind of sets a foundation for hopefully this to be replicated at different schools across the United States.”
NCOHC, a Foundation for Health Leadership & Innovation program, works to advance systems-level changes, improving the overall health and well-being of all North Carolinians by increasing access and equity in care. Sign up for our monthly newsletter to join the network and get involved!
Related NCOHC Blog Posts
- Racism, Food, and Your Mouth: Parallels Between Food and Oral Health Equity
- How the World Around Us Impacts Our Oral Health: An Intro to the Social Determinants of Health
- Social Determinants of Health: How the World Around Us Impacts our Mouths
- Social Determinants of Health – Structural and Governmental Influences

Dental cavities and gum disease remain the two most common oral health conditions—and they are often preventable. Cavities are also the most widespread chronic childhood disease and can continue into adulthood. Dental decay and other oral diseases at any age impact quality of life, school and work performance, and ability to access various opportunities.
In addition to increasing the availability of school-based preventative oral health services, policy changes, such as expanding the scope of practice laws for dental hygienists, have been shown to increase access to care and improve outcomes for children.
According to the North Carolina Department of Health and Human Services (NCDHHS) Division of Public Health Oral Health Section’s The Tragic Truth: Children’s Oral Health Declines in NC Post-COVID report, school-based services may be the only option to access dental care for children who are most at risk for developing oral disease in North Carolina.1
Find out how the ongoing impact of the COVID-19 pandemic and what the report revealed about the state of oral health for North Carolinian children.
Lack of Access to Oral Health Services During the COVID-19 Pandemic & Beyond
During the COVID-19 pandemic, the American Dental Association (ADA) recommended that dental practices postpone optional dental procedures like routine cleanings to decrease the likelihood of spreading the virus. According to an ADA Health Policy Institute survey, in March 2020, 76 percent of dental offices surveyed were closed for everything except emergency services, 19 percent were fully closed, and 5 percent were seeing fewer patients.2
While closures were necessary at the beginning of the pandemic to protect patients and providers, we continue to see the negative effects of this prolonged period of dental practice closures and limited school-based oral health services on children and communities.
Ongoing & Exacerbated Racial & Socioeconomic Disparities in Oral Health
Oral disease continues to disproportionately impact certain racial and ethnic groups. According to the Centers for Disease Control and Prevention (CDC), “non-Hispanic Blacks, Hispanics, and American Indians and Alaska Natives generally have the poorest oral health of any racial and ethnic groups in the United States.”2
Overall, only 39 percent of children from families with lower incomes and those at higher risk of cavities have received dental sealants compared with 46 percent for children from families with higher incomes.2
The Tragic Truth Report by the NCDHHS Oral Health Section
A key role of the North Carolina Oral Health Section (OHS) is to monitor community oral health across the state. In November 2023, Jessica Scott-Jeffries, DHSc, RDH School Oral Health Coordinator and Osaremhen Ikhile, BDS, DrPH Oral Epidemiologist from the NCDHHS Division of Public Health Oral Health Section published their research findings in The Tragic Truth: Children’s Oral Health Declines in NC Post-COVID.
Annually, the Public Health Oral Health Section collects oral health data on kindergartners using the Basic Screening Survey (BSS). Oral health indicators used in the survey include:
- Untreated decay,
- Treated decay, and
- No decay experience.
The first two indicators help determine “how well communities can access and use dental services,” while the third indicates “how well the overall oral health system and other determinants of health support optimal oral health of communities.”
NC Children’s Dental Health Statistics Post-COVID-19 Pandemic
The NCDHHS Division of Public Health Oral Health Section found:
- Untreated tooth decay in children is the highest it has been in five years.
- Treated decay in children is the lowest it has been in five years.
- No decay experience in children is the lowest it has been in five years.
Racial Disparities in Children’s Oral Health
In North Carolina, there has been a…
- 3-fold rise in untreated tooth decay among Native Hawaiian/Pacific Islander kindergartners compared to Asian kindergartners with no increase in untreated decay.
- 2.5x decrease in treated decay among Native Hawaiian/Pacific Islander kindergartners.
- American Indian/Alaskan Native and Asian kindergartners had less treated decay.
- 2.5x decrease in treated decay among Native Hawaiian/Pacific Islander kindergartners.
- American Indian/Alaskan Native and Asian kindergartners had less treated decay.
Poor oral health significantly impacts overall health and these systemic oral health disparities must stop. Not receiving the oral health care that they need and deserve can negatively impact children throughout their entire lives.
Two important steps to address the negative effects of the pandemic we continue to see today include 1) increasing access to preventative oral health services through school-based programs and 2) scope of practice policy changes essential.
To learn more, read The Tragic Truth: Children’s Oral Health Declines in NC Post-COVID.
1The Tragic Truth: Children’s Oral Health Declines in NC Post-COVID
2Oral Health and COVID-19: Increasing the Need for Prevention and Access
NCOHC, a Foundation for Health Leadership & Innovation program, works to advance systems-level changes, improving the overall health and well-being of all North Carolinians by increasing access and equity in care. Sign up for our monthly newsletter to join the network and get involved!
NCOHC’s 2023 in Review

As we step into 2024, we’re taking a moment to reflect on 2023 as we begin building on what we accomplished last year.
What a year 2023 was… Among many other headlines, one of the biggest for North Carolina was the passage of Medicaid Expansion, which finally went into effect statewide on December 1st. After more than a decade of advocacy from across our state, approximately 600,000 people who were living in the health care coverage gap are newly eligible for no- or low-cost health care.

2023 was also a big year for the North Carolina Oral Health Collaborative (NCOHC) and our incredible coalition of oral health advocates. NCOHC transitioned to new leadership as Dr. Steve Cline took over as the Vice President for Oral Health at the Foundation for Health Leadership and Innovation (FHLI) and Crystal Adams was promoted to the Director of NCOHC.
As we look back at what we achieved together, we are also thinking about how we will continue to advance oral health equity in 2024 and beyond.
We are thrilled to announce that we received our largest ever grant–$1.8 million over two years—from the Blue Cross and Blue Shield of North Carolina Foundation. This will support our work influencing policy, developing and promoting workforce strategies, elevating partnerships, and engaging with communities across North Carolina.
Moreover, it will enable us and our partners to advance the recommendations from the North Carolina Institute of Medicine (NCIOM) Oral Health Transformation Task Force Report.
We are also delighted to announce that The Duke Endowment—a longtime partner and supporter of our collaborative work—has continued to invest in oral health equity by awarding NCOHC a $1.2 million grant over the next three years. We are also grateful for the ongoing support of the Dogwood Health Trust and the CareQuest Institute.
With this funding secured, we will expand our programs and support a more accessible, equitable oral health ecosystem, especially for rural and other underserved communities across our state.
Read about our collective successes with our statewide partners and get a sneak peek of what’s to come in 2024.
2023 Legislative Breakfast
At the North Carolina Museum of History on April 26, 2023, the North Carolina Rural Health Association (NCRHA) and NCOHC, along with our partners and numerous legislators, met to discuss ways to address the growing health care needs of all North Carolinians.
We presented awards to impactful state leaders, including Representative Donna McDowell White (NC House District 26), Senator Jim Burgin (NC Senate District 12), Senator Jim Perry (NC Senate District 2), Dr. Amanda Stroud (Dental Director, AppHealthCare), and Michelle Fortune (CEO, St. Luke’s Hospital).

Additionally, NCOHC announced its legislative priorities for the 2023-2024 legislative session, which include:
- Enacting a state budget to allow House Bill 76 (Medicaid Expansion) to take effect — we did it!
- Creating a Rural Areas Forgivable Loan Pilot Program to encourage dentists, hygienists, and assistants trained in North Carolina to stay and bring more providers to rural communities by adding funding for dental staff loan forgiveness.
- Promoting legislation to allow all dental staff to practice at the full scope of their training and licensure (e.g., removing regulatory burdens for hygienists and assistants).
Along with that, the North Carolina Rural Health Association, another FHLI program, announced its 2023 legislative priorities, which included 1) Medicaid Expansion and access to care, 2) health workforce pipeline, 3) maternal and child health, and 4) broadband for all.
Oral Health Day 2023: Challenges and Opportunities for the Dental Team
On June 21, 2023, we hosted Oral Health Day 2023. The theme for this year’s event was, “Challenges and Opportunities for the Dental Team.” Kathy Colville provided a keynote speech and panelists brought expertise and ideas for how North Carolina can become a healthier, more equitable state.
“We have truly amazing and exceptional people holding up an inadequate system,” said Colville, President and CEO of the North Carolina Institute of Medicine (NCIOM). She also spoke about the necessity of a systems-level approach to improving oral health and how integral oral health is to many meaningful aspects of our lives:
“The mouth communicates, eats, smiles, frowns, and makes silly faces. Our mouth and teeth allow us to show emotion, communicate our thoughts, and be human. With proper oral health, our mouth can do all of these things better.”
Other key topics discussed throughout the day included 1) Medicaid Expansion and dental reimbursement rates, 2) building community trust, and 3) advocating for and investing in an adequate, accessible, and equitable oral health care delivery model throughout North Carolina.
We hope you will join us for Oral Health Day 2024, which will be announced soon!
Community Oral Health Transformation (COrHT) Wrap-Up Convening
In October we joined forces with the Blue Cross and Blue Shield of North Carolina Foundation and the CareQuest Institute for Oral Health to host a final COrHT Initiative convening. The two-year initiative launched in 2022 to help safety-net practices pilot a value-based care payment model, following CareQuest’s “three-domain framework” that includes:
- Tele-prevention (teledentistry)
- Minimally invasive care (non-surgical treatment of disease)
- Integration of oral health with overall health care
The initiative was so successful that we are excited to announce it will continue to live on! 2023 was originally intended to be the final year of the initiative, but at the 2023 convening every participating site agreed to stay involved and keep the initiative going.
We look forward to continuing to collect data, coach providers, and help explore avenues to transition to a value-based oral health system.
Western North Carolina (WNC) Oral Health Convening
We facilitated a WNC Oral Health Convening at the Lake Junaluska Conference Center in Waynesville this year with support from the Dogwood Health Trust. Dedicated oral health leaders working directly in small towns and rural communities throughout the Appalachian region came together for an engaging discussion about access to care, the current dental workforce, and policy priorities.
Following the sale of Mission Hospital to HCA Healthcare, NCOHC stepped in to help continue the convening of a WNC Steering Committee that formerly worked through the Mission Hospital Children’s Dental Clinic.
The goals of the committee and ongoing convenings are to 1) increase health care integration by facilitating collaboration among dental, medical, and public health providers, 2) expand access to oral health care for rural and other underserved communities, and 3) enhance oral health literacy for families, policymakers, and providers, and more.

Oral Surgery Mini-Residency in WNC
NCOHC partnered with the Mountain Area Health Education Center (MAHEC) to launch a mini-residency program at their WNC facilities. The goal was to better equip oral health safety-net providers in the region with the skills to meet people’s comprehensive oral health care needs, rather than referring them to an outside specialist.
The first cohort of four safety-net dentists received hands-on complex surgeries training. There is a severe shortage of specialty and surgical oral health care available to uninsured North Carolinians or those with Medicaid insurance. By “training up” already qualified providers in safety-net settings, people who would otherwise be left without options will be able to access the care they need and deserve.
Patient Advocate Pilot Program
This year marked year two of the Patient Advocate Pilot Program. Four dental practices in the WNC region hired patient advocates, employees who help people navigate the system and access the entire spectrum of health services, including oral health care.
NCOHC provided training and ongoing support, and we are continuing to collect data from the patient advocate pilot. Ultimately, we will use this information to analyze the effectiveness of the program, which will wrap up in 2024.
Participating sites include Mountain Community Health Partnership, Blue Ridge Health, MAHEC Dental Health Center and Center for Advanced Training, and the ECU Community Service Learning Center in Sylva, North Carolina.
2024 Preview: What to Expect
NCIOM Oral Health Transformation Task Force Recommendations
In January 2022, NCIOM and NCOHC launched the Oral Health Transformation Initiative, a multi-sector task force to evaluate, assess, and make oral health system transformation recommendations. More than 70 key oral and health care stakeholders, policymakers, academics, and other influencers have contributed through collaborative design to identify critical oral health opportunities in North Carolina.
The task force will release an Oral Health Transformation Task Force Recommendations Report by February 2024. The report will cover issues ranging from payment and benefit design to care integration, pathway development, and consumer experience. It will also lay out a path forward to implement key policy priorities to improve access and equity in oral health care across North Carolina.
Portrait of Oral Health Report
As we have done in the past, NCOHC engaged with UNC-Chapel Hill MPH capstone students throughout the year, enabling them to gain hands-on experience synthesizing data and interviewing key stakeholders to develop an informative report about the status of oral health in North Carolina.
This year, a group of four students are still dedicating their time, energy, and talent to put together the Portrait of Oral Health 2024. This report will be an updated version of the original Portrait of Oral Health [PDF] published in 2017 by a group of oral health professionals, government officials, and community-based organizations.
Join Us on the Road to More Equitable Oral Health Across NC
With 2023 swiftly falling into our rearview mirrors, we feel deeply grateful for the dedicated partnerships and collaborative efforts we have had the privilege to be part of. As we enter a new year, we feel excited about embarking on the open road ahead together.
Our team will continue to advocate for and advance policies and initiatives that create a healthier, more equitable oral health landscape for every North Carolinian. Stay tuned for details about events like this year’s Legislative Breakfast and Oral Health Day.
NCOHC, a Foundation for Health Leadership & Innovation program, works to advance systems-level changes, improving the overall health and well-being of all North Carolinians by increasing access and equity in care. Sign up for our monthly newsletter to join the network and get involved!

Medicaid Expansion finally took effect statewide on December 1st, 2023, thanks to over a decade of advocacy by countless organizations and individuals. All of us here at NCOHC and the Foundation for Health Leadership & Innovation (FHLI) are thrilled to see this important step forward for North Carolina take effect, but we will also continue working hard to improve health access and equity for all North Carolinians.
Medicaid Expansion is expected to provide over 600,000 people in the health care coverage gap, including veterans, frontline workers, small business owners, parents, and many more, with access to health insurance. This includes residents with incomes too high to qualify for Medicaid but too low to receive health care subsidies through the Affordable Care Act marketplace.
This insurance will include comprehensive health coverage, including dental, behavioral health, and vision care.
Find out whether you may be eligible for benefits and what Medicaid Expansion means for rural and other underserved communities across our state.
FAQs About Medicaid Expansion in North Carolina
Here are answers to some frequently asked questions about Medicaid Expansion in North Carolina effective December 1st, 2023:
Who is eligible for Medicaid Expansion in NC?
Most adults ages 19-64 who earn up to 138% of the federal poverty line (e.g., singles earning about $20,000/year or families of three earning about $34,000/year) may be eligible. Read more about eligibility requirements.
How can I apply for Medicaid in North Carolina?
Applying online through ePASS is the quickest option. For a step-by-step tutorial, watch this how-to YouTube video from the NC Department of Health and Human Services (NCDHHS). You can also apply in person, by phone, or by mail.
How long will it take for my Medicaid application to be processed?
It may take up to 45 days (about 1 and a half months) for your application to be processed. Apply today to access your benefits as soon as possible.
What does Medicaid health coverage include?
Medicaid includes primary care, hospital stays, maternity care, vision and hearing, dental/oral health care, and more.
What does Medicaid pay for?
Full Medicaid health care coverage pays for your doctor visits, yearly check-ups, emergency care, mental health, and more. There are no monthly fees and copays are never more than $4.
What Medicaid Expansion Means for Rural & Underserved Communities in NC
The 2023 North Carolina Rural Health Snapshot [PDF] report compiled by the North Carolina Rural Health Association (NCRHA), an FHLI program, shows that rural residents are 40% more likely to be uninsured and eligible for Medicaid Expansion.
It is expected to create an estimated 37,200 jobs, generate thousands in savings for small businesses, and bring billions of dollars in federal funding back to North Carolina annually. In addition to strengthening our economy, it will help our communities become more resilient and increase access to timely, affordable health care.
According to the NCRHA’s sweeping analysis, previous studies also show that Medicaid Expansion is associated with improved hospital financial performance and fewer hospital closures. Since 2010, when Medicaid Expansion first became an option for every state, seven rural hospitals have closed in North Carolina. We need to rebuild and expand the rural health infrastructure to effectively serve our rural and other historically underserved communities.
As hundreds of thousands of people gain access to coverage through Medicaid Expansion, we must continue to work at every level to create a more accessible and equitable health care system. This means expanding the number of culturally competent providers who accept Medicaid insurance for all types of care, including oral health and specialty services.
Stay Tuned for More on Medicaid Expansion in North Carolina
FHLI and all our programs will continue to advocate for all North Carolinians and leverage policies that increase health care access and equity across our state. While Medicaid Expansion is an important win expanding access to care across our state, much work will still need to be done to ensure those who gain coverage have access points to receive quality care.
Follow us on social media and sign up for our newsletter to stay up to date about Medicaid Expansion.


