At NCOHC and the Foundation for Health Leadership & Innovation (FHLI), we are reflecting on 2019 and planning for 2020. Here are our highlights from last year and our plans for the year ahead.

What NCOHC Accomplished in 2019
In 2019 we supported communities across North Carolina, helping local leaders build relationships and collaborate with provider networks, educators, and more, to positively impact oral health outcomes.
We increased NCOHC’s educational impact, piloting an oral health practicum experience with Campbell University public health students and leading roundtable sessions at the UNC Gillings School of Global Public Health. Director Dr. Zachary Brian spoke at more than 40 workshops and presentations across North Carolina and around the country.
On the policy front, NCOHC worked hard to develop a fruitful partnership with the North Carolina Dental Society (NCDS). Together, we sponsored a regulatory rule change that will allow dental hygienists to practice to the full extent of their licensure, a change that will expand access to affordable health care for those who need it most.
Stay tuned, as the rule change is expected to be approved by the Rules Review Commission later this month!
Finally, with help from the oral health and policy advisers who make up our Collaborative Acceleration Team (CAT), NCOHC developed a Strategic Plan, setting ambitious goals to guide our work for the next five years.
be sure to check out our full Year in Review in NCOHC’s December Newsletter.
What We’ll Do in 2020
With guidance from our Strategic Plan, NCOHC will hit the ground running in the new year. We expect to see the regulatory rule change that we co-sponsored with NCDS signed into effect in the next few weeks, and we will continue to positively impact the oral health of North Carolinians through state-level advocacy.
We will continue to work with communities across the state to help local leaders increase access to oral health care. We will provide resources to these leaders, oral health care providers, and to the general public, and we will leverage our newly expanded capacity to increase NCOHC’s organizational effectiveness
stay tuned to our developing Resource Center—part of our newly redesigned website—for the latest oral health news and information for providers, policymakers, and the public.
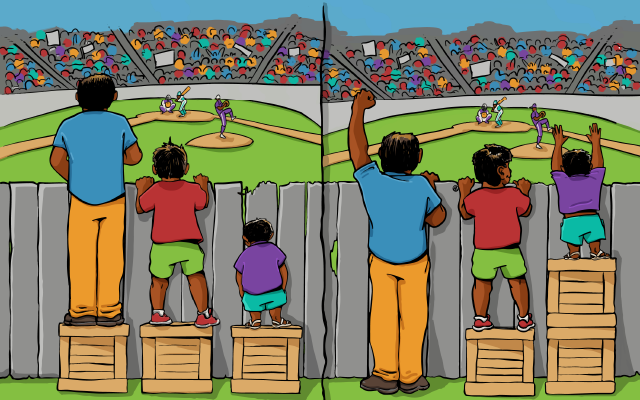
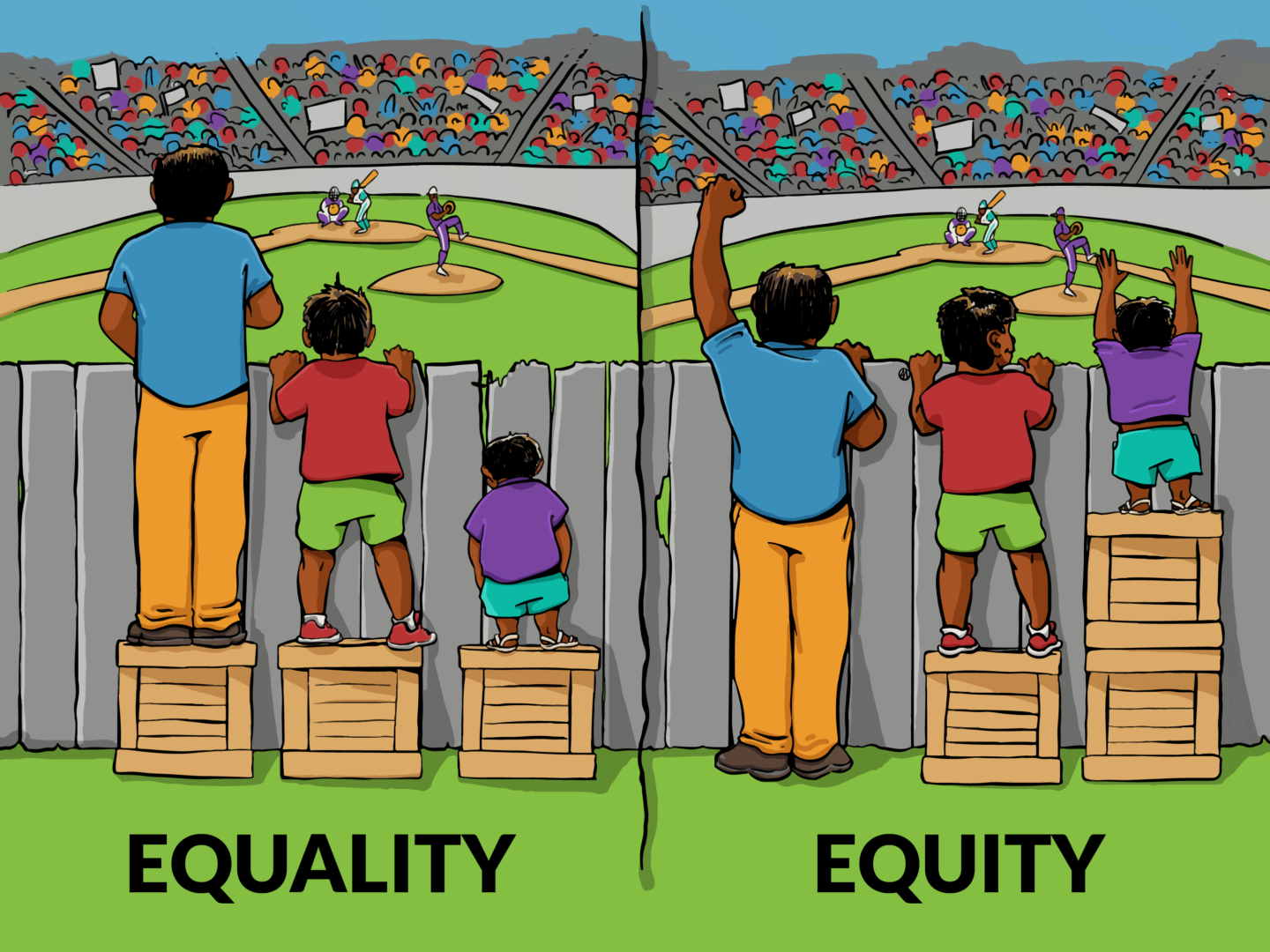
All our work will impact NCOHC’s overall goal of advancing systemic change in oral health care. Our aim is to promote a value-based approach, recognize social determinants of health and barriers to equitable oral health care, and promote solutions to create an equitable landscape for all North Carolinians.
These are Our Oral Health Care Resolutions for 2020. What are Yours?

NCOHC is a program of the Foundation for Health Leadership & Innovation (FLHI). For more information and to stay up to date, subscribe to the NCOHC Newsletter. If you are interested in becoming an NCOHC member, you can also fill out our membership form. It’s free!