The North Carolina Public Health Association recently hosted its 2020 Public Health Leaders’ Conference, drawing professionals from across North Carolina to discuss pressing issues and the public health landscape as we look ahead to 2030 and beyond.
In many ways, this year’s conference marks a turning point in North Carolina, so we sat down with Foundation for Health Leadership & Innovation President and CEO Anne Thomas to talk about the conference and her takeaways.

The theme of the 2020 Public Health Leaders’ Conference was “Shifting the Trajectory: Advancing Equity in Public Health.” According to Thomas, the importance of equity is not a new concept in public health, but the unified focus across public health leaders in North Carolina marks a promising change.
Putting Health Equity Front and Center
“We haven’t always spoken with the language of equity,” said Thomas. “I became a public health director in 1996, and we always talked about disparities, but the conversations used to be, ‘If we just tell people to change what they eat and how they live, they will be healthier.’ We can tell people how to be healthy, but if they don’t have insurance, transportation, or the proper food, and if we don’t address root causes like structural racism and poverty, we aren’t really going to make much of a difference.”
Thomas said that the intentional shift toward an equity-focused landscape in public health is significant. While disparities in health have always been a top priority for public health leaders, the focus has generally been from a clinical frame, leaving non-medical drivers like food, transportation, and housing out of the picture.
At the conference, the North Carolina Institute of Medicine (NCIOM) and the North Carolina Department of Health and Human Services (DHHS) unveiled their “Healthy North Carolina 2030” strategy, which lays out priorities to improve health in the new decade.
The focus on health equity and the overall drivers of health outcomes speaks to the new transformational vision for public health in our state to improve the health and well-being of all North Carolinians.
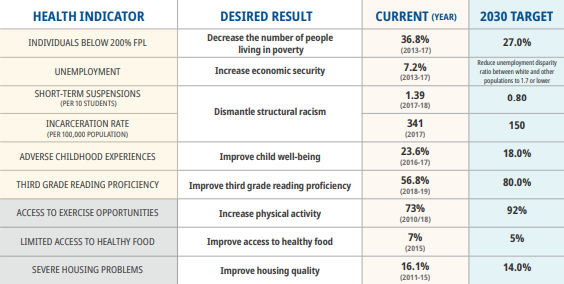
This excerpt from “Healthy North Carolina 2030” highlights non-medical factors like incarceration rate, reading proficiency, and suspensions as important indicators of health.
Using Social Determinants of Health to Understand Equity
Want to Know More About Social Determinants of Health?
Read our analysis of the most pressing systemic barriers to access where we break down how geography, income, language, race, and more can impact health outcomes.
To highlight health inequities, speakers at the conference discussed the importance of understanding and tackling non-medical drivers of health. Instead of simply treating patients, the speakers championed a more encompassing approach, understanding that health starts in homes, schools, and communities, not once you walk through the doors of a doctor’s office.
“The thing that has really changed is that we are talking about the non-medical drivers of heath, the root causes that have caused health inequities, and evidence-based strategies to address them,” said Thomas.
Thomas said that 20 percent of a person’s health is the result of clinical care, and 80 percent comes from other factors known as social determinants of health. To address that 80 percent, providers will pay attention to social determinants of health, and the health care systems will provide mechanisms to make things like food, housing, and transportation accessible to those who need them to be healthy.
Buying Health: Equity in Action
The concept of “buying health” is where equity becomes operationalized. Buying health refers to a value-based model where health outcomes are measured and paid for, versus the current fee-for-service model, where the cost of care is determined by the service(s) provided.
“Right now, if I go to the doctor, the office gets paid. It doesn’t matter if my health improves because there was an office visit,” said Thomas. “The concept of buying health means screening for these non-clinical factors, and if it is food that they need, or transportation, that food or transportation will actually be paid for.”
NCCARE360, a partnership between FHLI and the Department of Health and Human Services, was also an important topic of conversation at the conference, specifically regarding buying health. NCCARE360 is the first statewide network to unite health care and human services, using shared technology to coordinate person-centered care that provides for both medical and non-medical needs.
By the end of 2020, NCCARE360 will be available in all 100 counties in North Carolina.
Thomas said that buying health was an important topic at the conference, especially as North Carolina prepares for Medicaid Transformation, the state’s plan to transition from Medicaid’s fee-for-service model to “Medicaid Managed Care.” Under Managed Care, the state government will work with insurance companies to create a system that incorporates physical and behavioral health to address both the clinical needs and social determinants of health for Medicaid recipients.
“I feel like we are at a tipping point now,” said Thomas. “Equity is no longer something we just talk about. We are developing real strategies to achieve it.”
Our Oral Health Takeaways
The major themes of this conference—implementing equity, understanding social determinants of health, and transitioning towards value-based care—all apply to oral health care as well as traditional medical care. In fact, these new points of focus highlight the importance of breaking down the siloes that traditionally separate oral health from the rest of the body.
“This new focus is helping communities and providers realize that we really can’t separate the head from the mouth from the body, and we need to stop thinking in a siloed mentality,” said Thomas.
At NCOHC we believe that integrated care models that address all of a patient’s needs, incorporating oral health, medical health, and non-medical needs all under one roof, are integral in creating an equitable health future for all North Carolinians.
As we head into 2020 and plan for the decade ahead, we are excited to work hard to address social drivers of health and pave an equitable path to a healthier future for all North Carolinians.
NCOHC is a program of the Foundation for Health Leadership & Innovation. For more information and to stay up to date, subscribe to the NCOHC newsletter. If you are interested in becoming an NCOHC member, you can also fill out our membership form. It’s free!