Last week, FHLI’s North Carolina Oral Health Collaborative travelled with North Carolina oral health leaders to Charleston, South Carolina, for a tour of the Medical University of South Carolina’s (MUSC) Telehealth Center of Excellence.
Front row, left to right: Shaun Matthews, DDS, MD (UNC Adams School of Dentistry); Crystal Adams, MA, CDA, RDH (Catawba Valley Community College); Nancy St. Onge, RDH (NC State Board of Dental Examiners)
Second row, left to right: Mark Casey, DDS, MPH (North Carolina DMA); Zachary Brian, DMD, MHA (NCOHC)
Third row, left to right: Kelsey Ross Dew, MPH (NCOHC); Lisa Ward, CAE (NC Dental Society).
The MUSC Telehealth Center of Excellence, one of only two HRSA-designated sites in the U.S., is home to state-of-the-art facilities, including an impressive array teledentistry technologies. To help North Carolina’s oral health leaders understand teledentistry and how the technology can benefit patients in our state, the group toured the facility and spoke with leading medical providers and dentists at the forefront of innovations in telehealth.
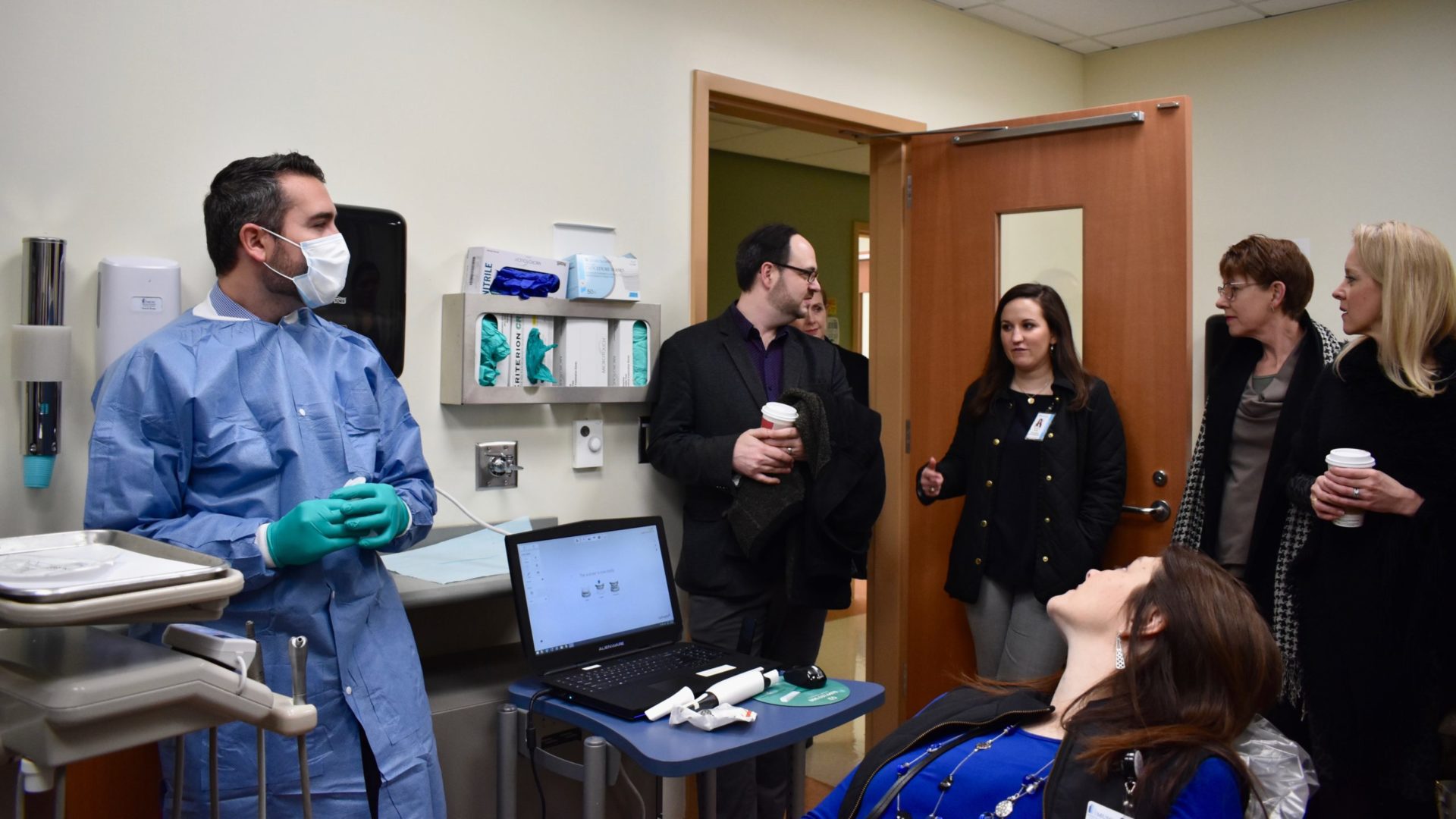
Dr. Walter Renne demonstrating cutting edge intraoral camera technology to the tour group.
Dr. Walter Renne, Assistant Dean of Innovation and Digital Dentistry at MUSC, demonstrated the process of scanning a patient’s teeth via an intraoral camera, one of the key tools of teledentistry.
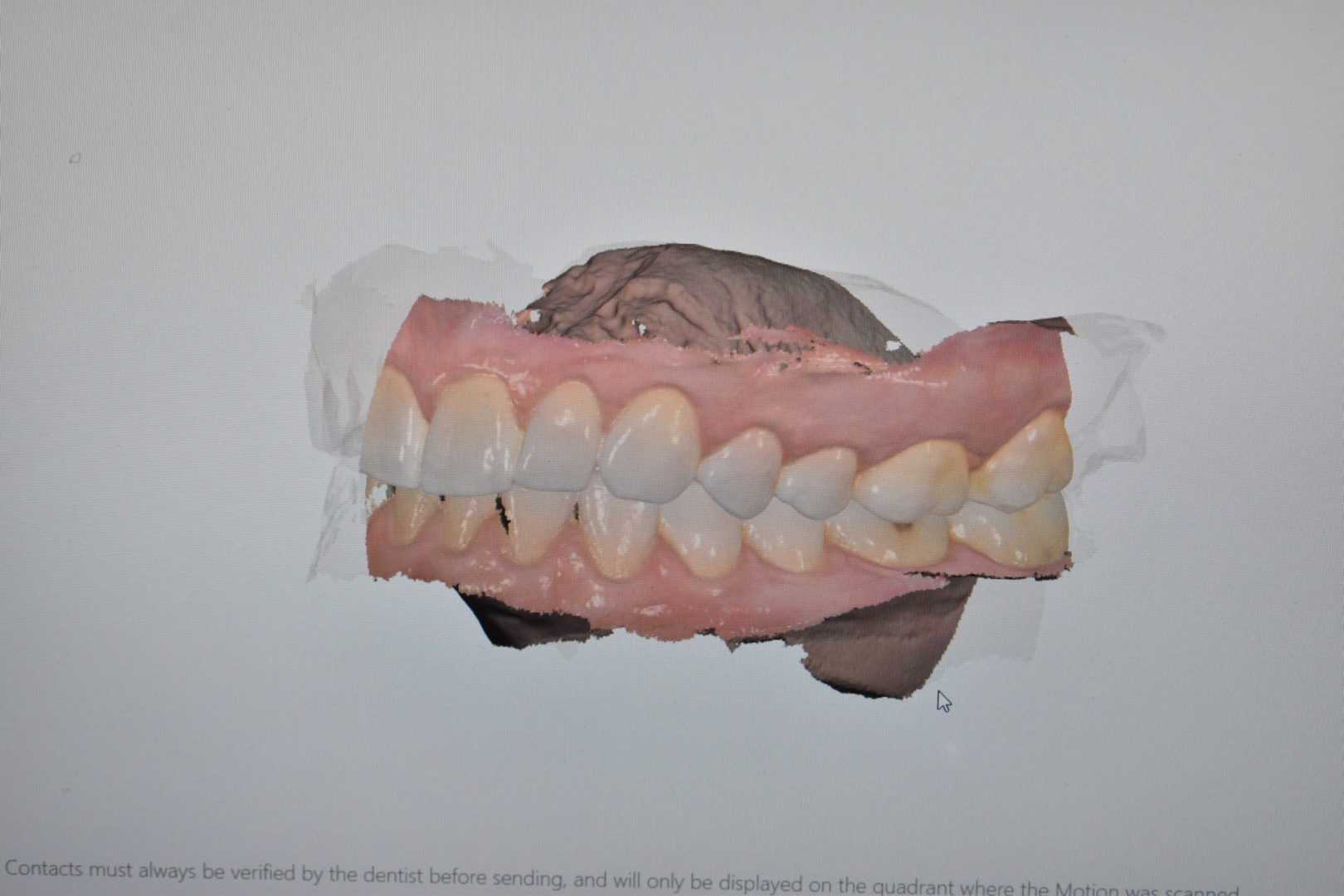
The camera that Dr. Renne used can produce a 3D image of the patient’s teeth, and it can even render the gums as well. The scan produced can highlight potential points of decay to help a dental provider decide whether the patient needs further treatment or a more traditional in-person exam.
A 3D model of a patient’s teeth and gums created by an intraoral camera.
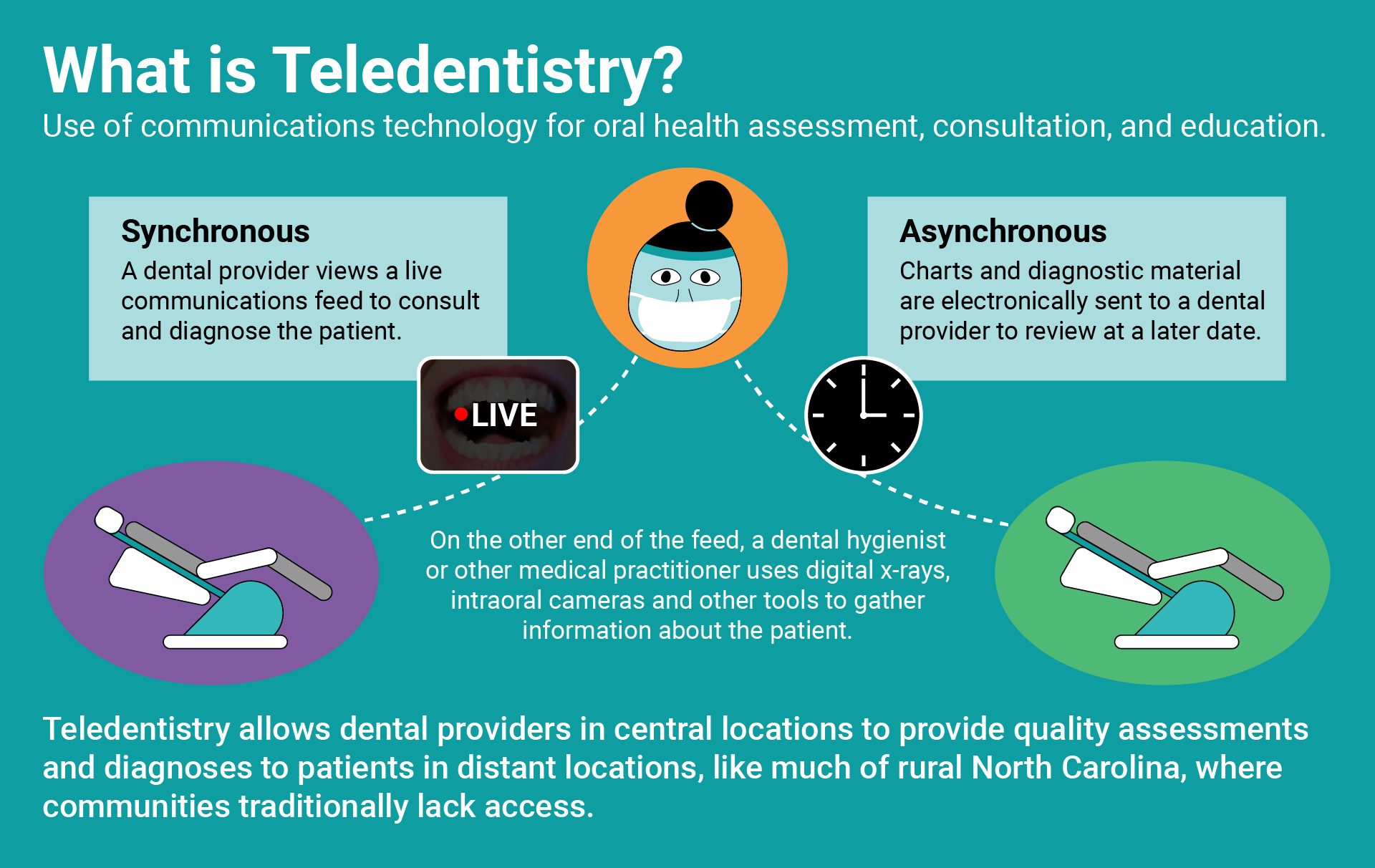
Unlike many fields of telehealth, teledentistry is a relatively affordable venture. The equipment required is minimal—primarily limited to a digital x-ray machine, an intraoral camera, and digital patient records (all of which are already used in many dental offices).
The MUSC tour group debriefing with MUSC leadership.
In addition, the telehealth services provided by MUSC extend far beyond just teledentistry. Patients across South Carolina can meet with doctors virtually for a wide variety of health services, from stroke and neurology care to psychiatry, pediatric care, and more.
Through its telehealth services, MUSC is able to reach patients in non-traditional settings such as schools, nursing homes, and correctional facilities—reducing costs and limiting time burdens on patients and care providers alike.
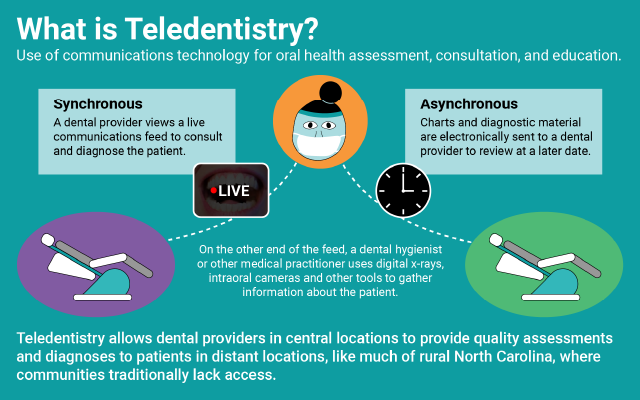
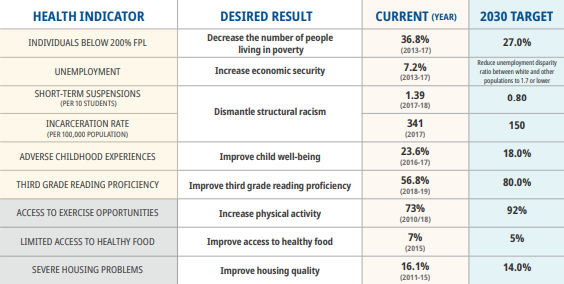
With 74 of North Carolina’s 100 counties designated as Dental Health Provider Shortage Areas (HPSAs), teledental services could make a significant impact in addressing access gaps. Teledentistry has the potential to increase access to basic oral health screening and diagnostic services in communities that disproportionately lack access to optimal oral health services.
While teledentistry is already used in a variety of settings, North Carolina’s regulatory framework limits its use from expanding into areas where it may be most impactful.
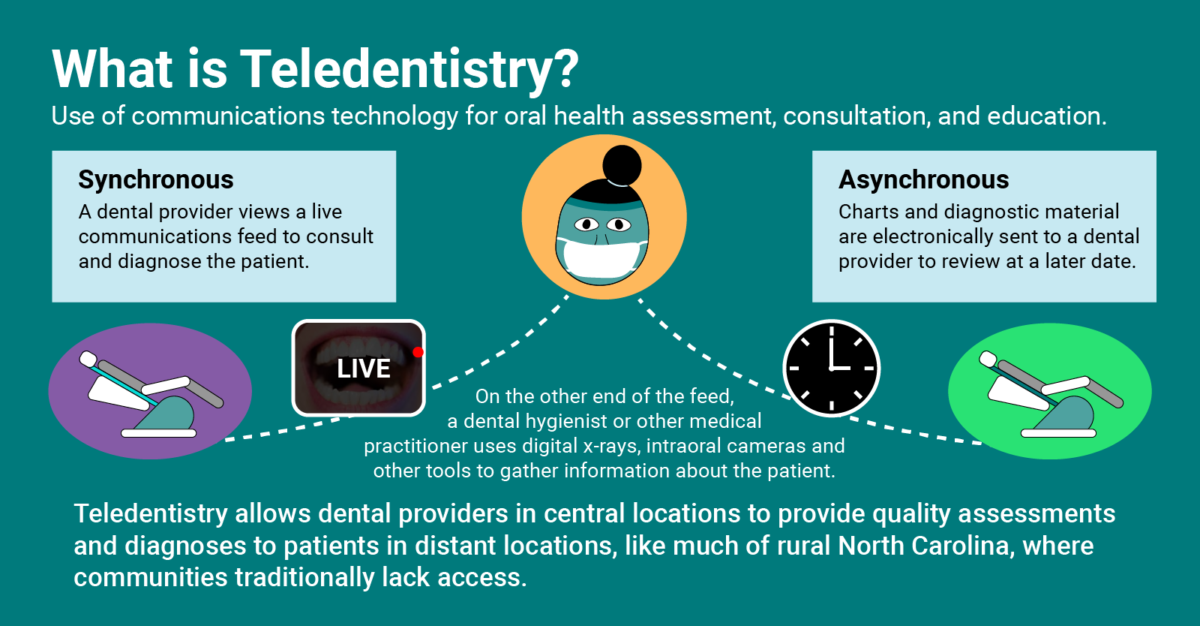
North Carolina’s Dental Practice Act, which regulates the practice of dentistry in the state, was written long before teledentistry was a viable opportunity for care. Additionally, a dentist who currently provides “synchronous” teledental care (i.e. live dental consultation, education, or examination provided in real-time) would be limited in their compensation. Equally as important, there currently is no reimbursement model for asynchronous teledentistry (i.e. “store-and-forward” care in which x-rays and other diagnostic information is taken and later reviewed by a dentist off-site).
That’s why this year, NOCHC’s Oral Health Day 2020 will focus on teledentistry and the opportunities it brings to North Carolina. Visit our Oral Health Day page to find out more about teledentistry’s potential in North Carolina, and register today!
Click here to see the rest of the photos from our trip to MUSC.
Sign up for NCOHC’s newsletter list to receive updates on stories like this one directly to your inbox.
NCOHC is a program of the Foundation for Health Leadership & Innovation. For more information and to stay up to date, subscribe to the NCOHC newsletter. If you are interested in becoming an NCOHC member, you can also fill out our membership form. It’s free!