We’d like to start off this blog post with a quote from the Terry Pratchett novel, “Men at Arms.” The book is a fantasy novel, but the quote underscores an important reality of poverty, that is, it is expensive to be poor.

Pratchett’s fictional “boots theory of socioeconomic unfairness” is a reality for many across North Carolina, and across America, today.
For example, the average washing machine uses 19 gallons of water per load. Accounting for the average cost of municipal water and electricity, running your own washing machine costs a mere 30 cents per load. Nationwide, however, laundromat patrons pay approximately $2.00 per load.
It is over six times more expensive to have clean clothes in America if you’re too poor to buy a washing machine. And that doesn’t even take into account the luxury of an electric clothes dryer.
Saving money is a luxury tied in many ways to wealth. If you have a little extra cash at the end of the month, you can invest your hard-earned dollars in stocks, property, or other means that allow those dollars to grow. You can make decisions to spend money up front that allow you to save down the road. For example, you can decide to spend an extra few thousand dollars on a newer, more efficient vehicle, saving money on gas and repairs in the long-run.
If you have mouths to feed and rent to pay, and you’re living paycheck-to-paycheck, you generally will end up spending more on basic necessities than you would if you had more economic flexibility.
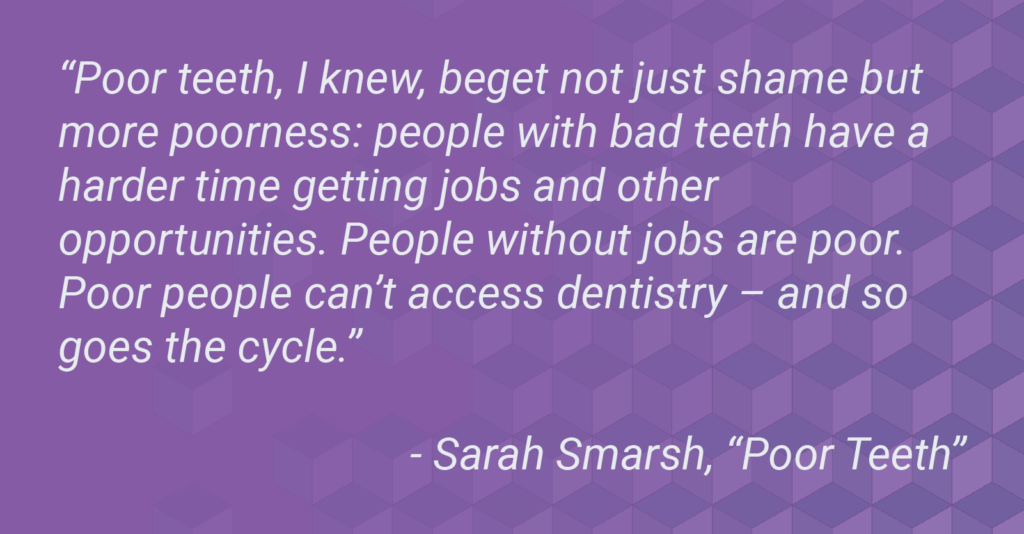
If you are poor in North Carolina, you are more likely to lack access to basic preventive care and oral health education as a child. As a result, you are more likely to experience tooth decay, both as a child and later as an adult.
Insurance aside, the average cost of one filling runs between $200 and $600.
For a root canal, average costs range from $700 for a front tooth up to $1,800 for a molar. Add the necessary crown following a root canal and you’re looking at an additional $300 – $3,000, depending on the crown’s material.
There are many options for low-cost dental care using sliding scales based on income, but at the end of the day, even one tooth with serious decay is much more expensive than an annual checkup and cleaning (especially with insurance, which generally covers the entire cost of routine preventive care).
Outside of the dental office, oral health takes an additional economic toll. How do you think a missing front tooth would impact your job prospects? Your confidence? Your ability to eat healthy foods?
North Carolinians visit emergency departments for oral care at twice the national rate. This particular statistic may be the most shocking, as the majority of hospitals are entirely unequipped to handle oral disease.
If you go to a hospital once you can’t handle the pain of your toothache any longer, you are likely to be prescribed an antibiotic and an opioid. Opioids are only a temporary fix for pain, and they bring with them a host of other potential problems. Antibiotics are not a solution for oral disease, either, but a temporary solution to potentially address the acute need. The pain and swelling may go away temporarily, but the root cause will still be in your mouth, potentially landing you back in the emergency department in a few months, with a new hospital bill.
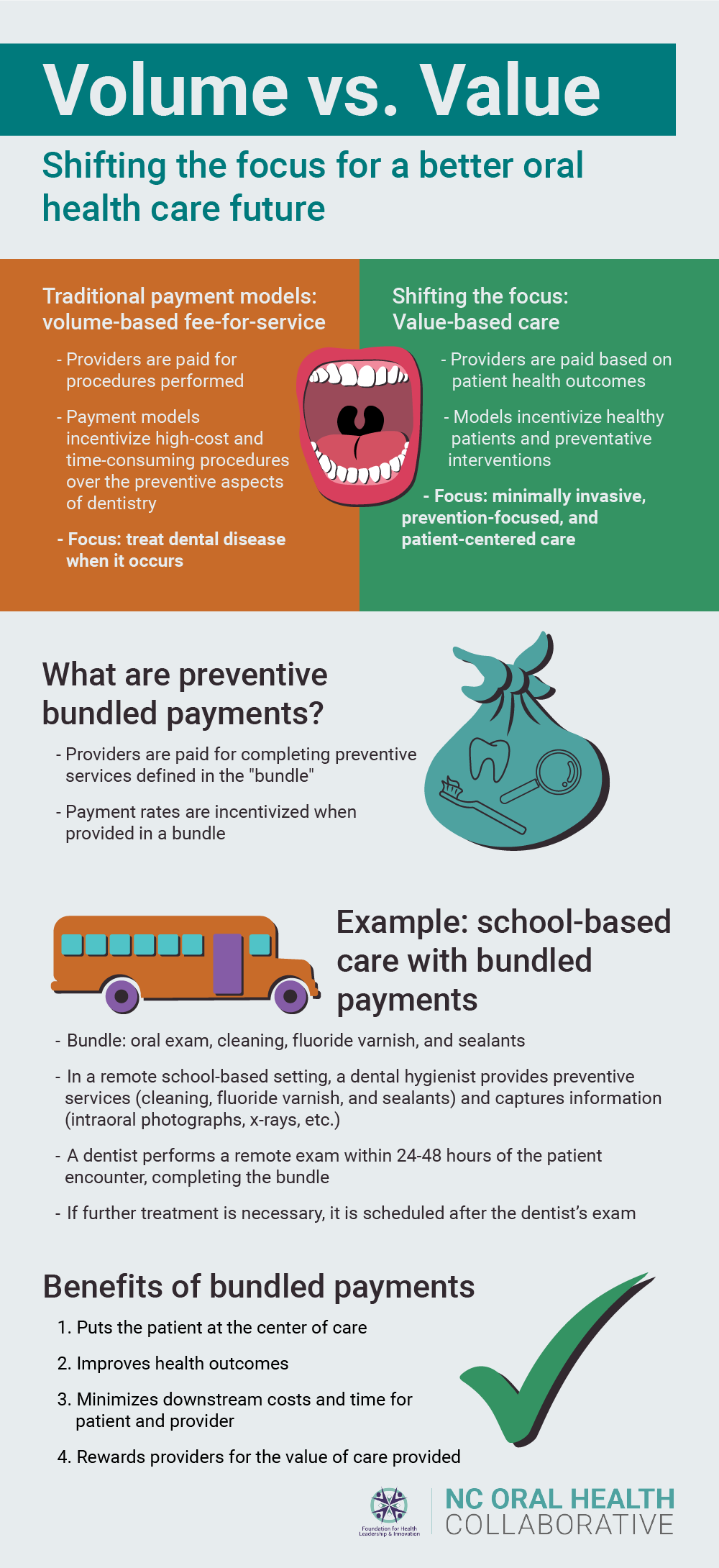
In the same way that individuals with economic flexibility can spend dollars up front to reduce costs down the road, systems can operate in a similar fashion. In oral health, and in health care in general, dollars invested in preventive care—spent up front and before issues emerge—can not only lead to the best health outcomes, but they can also create more economically sustainable systems.
We need to structurally change the oral health care system in North Carolina, ensuring that every single child and adult has access to quality preventive care and oral health education. Beyond being the right thing to do, it is a fiscally responsible move that will save both individuals and our state government money in the long run.
Oral health care price estimates were gathered from newmouth.com
NCOHC is a program of the Foundation for Health Leadership & Innovation. For more information and to stay up to date, subscribe to the NCOHC newsletter.