The connection between oral health and overall health is increasingly clear, but you wouldn’t know it looking at the federal government’s Medicare program. Medicare, which provided health insurance for more than 62 million U.S. retirees and people with disabilities in 2020, does not include dental coverage — except in very limited circumstances.
Overall, according to a 2019 study by the Kaiser Family Foundation (KFF), 47 percent of Medicare beneficiaries do not have dental coverage. While some Medicare beneficiaries have a dental benefit through optional, add-on Medicare Advantage plans (with additional premiums and co-pays), the scope of coverage is often extremely limited. For much of the older adult population in the United States, oral health care services are simply unaffordable.
A Public Health Emergency
The lack of Medicare dental coverage and high out-of-pocket costs facing older U.S. adults with oral health needs represent a true public health emergency. Forty-seven percent of Medicare beneficiaries did not have a dental visit in the last year, according to the same KFF study. The impact is especially disproportionate for marginalized communities, with the percentage without a dental visit climbing to 68 percent for Black beneficiaries, 61 percent for Hispanic beneficiaries, and 73 percent for low-income beneficiaries. Other at-risk populations are similarly affected. Among Medicare beneficiaries in fair or poor health, for example, the number is 63 percent.
The consequences are as devastating as they are preventable. A study by KFF of the 2016 Medicare Current Beneficiary Survey (MCBS) found that among all Medicare recipients living in the community, “18 percent have some difficulty chewing and eating solid foods due to their teeth.” This includes 29 percent of low-income recipients and 33 percent of recipients with disabilities under age 65. Oral health conditions are also common among the Medicare population: over 14 percent of older U.S. adults have untreated dental decay (caries), and 68 percent have periodontal disease (gum disease).
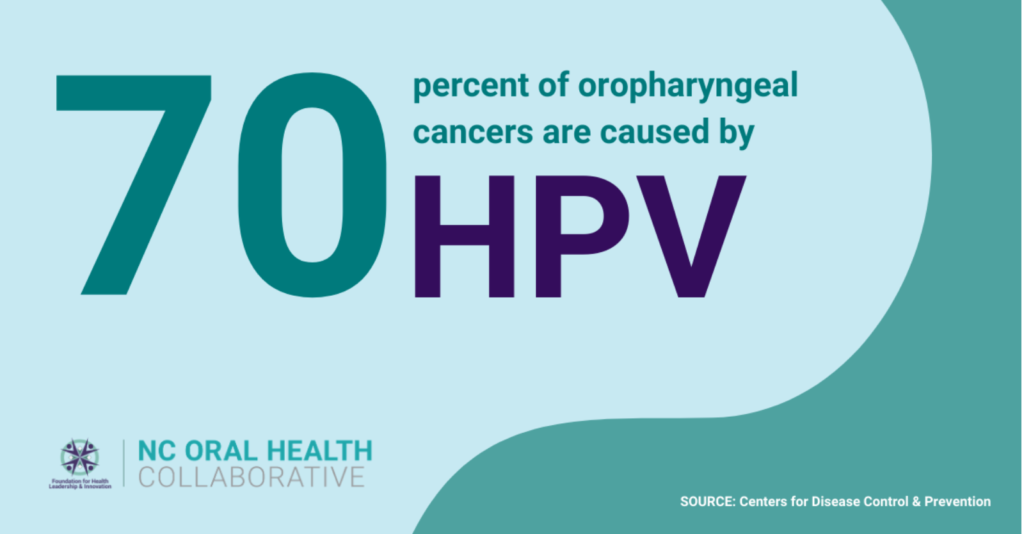
Various studies have linked periodontal disease to systemic health problems like diabetes, heart disease, kidney disease, and cancer. Dr. Lisa Simon and Dr. William Giannobile said it well in a recent opinion piece appearing in the New England Journal of Medicine: “The key reason that access to dental care is crucial is that, even in the absence of other medical complications, dental problems are a preventable and far-too-common source of disabling disease.”
That reality is especially true for older adults. “Growing evidence shows that poor oral health can worsen health conditions disproportionately impacting older individuals such as diabetes and cardiovascular disease — conditions that Medicare does cover,” the National Dental Association stated in a September letter calling for the expansion of Medicare to include a dental benefit.
A Historic Opportunity
In the decades since Medicare’s establishment in 1965, advocates have continually pushed for expanding the program to include dental, hearing, and vision benefits. However, current political realities mean that reform is perhaps closer than ever before. Powerful interest groups nevertheless threaten to dramatically scale back or derail the proposed change.
“Means-Testing” for Medicare Dental Benefits: A Costly Mistake
Despite not necessarily opposing a dental Medicare benefit altogether, some interest groups are applying the brakes. Rather than make dental coverage universal for all Medicare recipients, some have endorsed a model in which Medicare dental benefits would be available only to beneficiaries whose incomes are 300 percent or less of the federal poverty level (FPL), equating to roughly $38,000 per year for an individual.
To be clear: this would be a mistake. “Means-testing” has never been used with other health coverage under Medicare and would represent a step in the wrong direction if applied to a new dental benefit.
An Inequitable, Potentially Destabilizing Solution
By means-testing dental Medicare benefits, oral health care would remain out of reach for millions of working and middle-class older adults. That’s because out-of-pocket costs for dental care would still exceed many individuals’ available discretionary income, even for those earning more than 300% FPL. After all, KFF reports that out-of-pocket spending on dental care was $874 on average for Medicare beneficiaries using dental services in 2018 and that one in five Medicare beneficiaries using dental services spent more than $1,000 out-of-pocket. Many seniors, the majority of whom live on fixed incomes, simply cannot afford the out-of-pocket costs associated with routine, preventive dental care, to say nothing of more costly restorative or surgical procedures.
Beyond this inequity, however, means-testing dental benefits could potentially threaten the sustainability of the broader Medicare program. Max Richtman, president and CEO of the National Committee to Preserve Social Security and Medicare, noted in a recent op-ed that “If means-testing results in Medicare becoming increasingly unfair to higher-income beneficiaries, they may opt-out and purchase their policy on the private market. The departure of higher-income beneficiaries, who tend to be younger and healthier, would weaken the risk pool, putting additional strain on Medicare’s finances.” Further, as Richtman writes, applying the first-ever means-test to a Medicare benefit would set a dangerous precedent for future means-testing of other coverages.
Moreover, applying a means test to Medicare dental benefits would likely result in a situation in which a majority of private practice dentists decline to participate. We’ve seen this happen with Medicaid and the Children’s Health Insurance Program (CHIP). By limiting the potential pool of new patients, means-testing a Medicare dental benefit would similarly and significantly reduce the financial incentive for private practice dentists. According to the ADA Health Policy Institute (HPI), only 43 percent of dentists nationwide participate in Medicaid or CHIP, dramatically limiting access to care and fueling health disparities among disadvantaged populations. A means test applied to Medicare would almost certainly compound the problem.
The Bottom Line
Dental coverage under Medicare is sorely needed, but to make Medicare dental benefits anything but universal diminishes the message that public health-minded dentists have fought so hard to advance: that oral health is overall health. It also threatens to deepen inequities and deny care to at-risk populations that need it most. Congress should act now to expand Medicare to include dental coverage and reject misguided attempts to impose means-testing on potential beneficiaries.
Dr. Zachary Brian is the Director of North Carolina Oral Health Collaborative (NCOHC) and VP of Impact, Strategy, and Programs for its parent organization, the Foundation for Health Leadership & Innovation (FHLI).