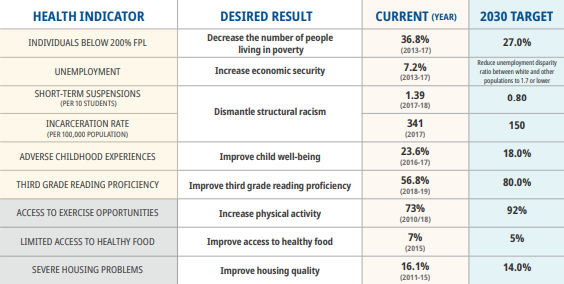
Recap: The Oral-Systemic Connection
Parts one and two of our series, “Healthy Mouth, Healthy Body,” focused on heart disease, diabetes, and how the two are linked to oral disease
Gum disease, or periodontal disease, can allow harmful bacteria to enter the bloodstream and cause chronic inflammation. This inflammation is linked to conditions like atherosclerosis, an artery disease that can lead to heart attacks and strokes.
Diabetes is connected to gum disease in several ways. Dry mouth caused by diabetes can lead to suboptimal oral health, and gum disease itself can increase the prevalence of risk factors for diabetes like elevated blood glucose levels
To catch up, be sure to read parts one and two of this series.
Healthy Mouth, Healthy Pregnancy
Even though this follows posts about heart disease and diabetes, to be perfectly clear, we are NOT calling pregnancy a disease! (And, brushing your teeth, well, cannot prevent pregnancy.)
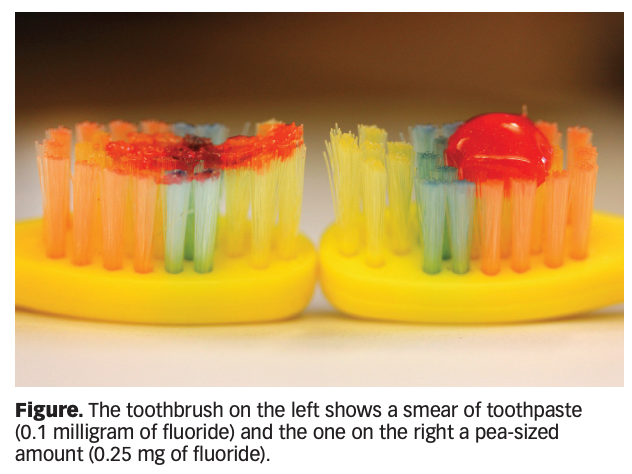
Pregnant mothers experience significant changes in their bodies during pregnancy, and some of these changes can impact oral health. For example, hormone imbalances can lead to gingivitis in the expecting mother. Increased vomiting from morning sickness, too, can increase the likelihood of developing cavities and tooth erosion (stripping of the tooth’s enamel).
Additionally, the research into the oral-systemic connection during pregnancy draws a connection between gum disease and low birthweight in newborns. Bacteria from gum disease can release toxins in the mother’s body that causes the body to produce chemicals that may stimulate contractions prematurely.
Research also reveals that gum disease may be linked to pre-term birth, but that connection is much less certain for now.
What Does This Mean?
For expecting mothers, it is important to work dental care into the already busy health care routine during pregnancy. For individuals who qualify for Medicaid while pregnant, NCOHC is working to support the extension of dental benefits post-partum to match perinatal health care coverage, which currently lasts 60 days after birth in North Carolina. You guessed it — currently, oral health coverage for the mother ends at time of delivery.
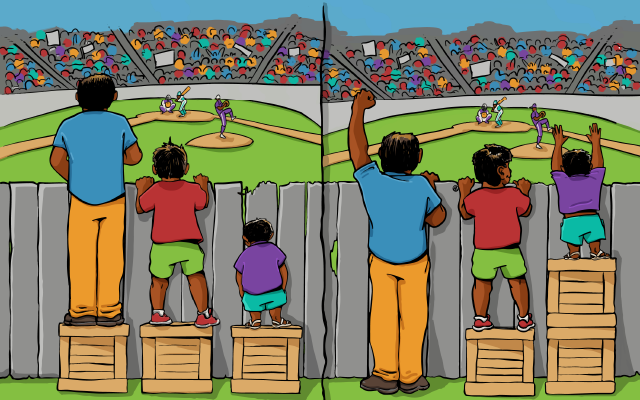
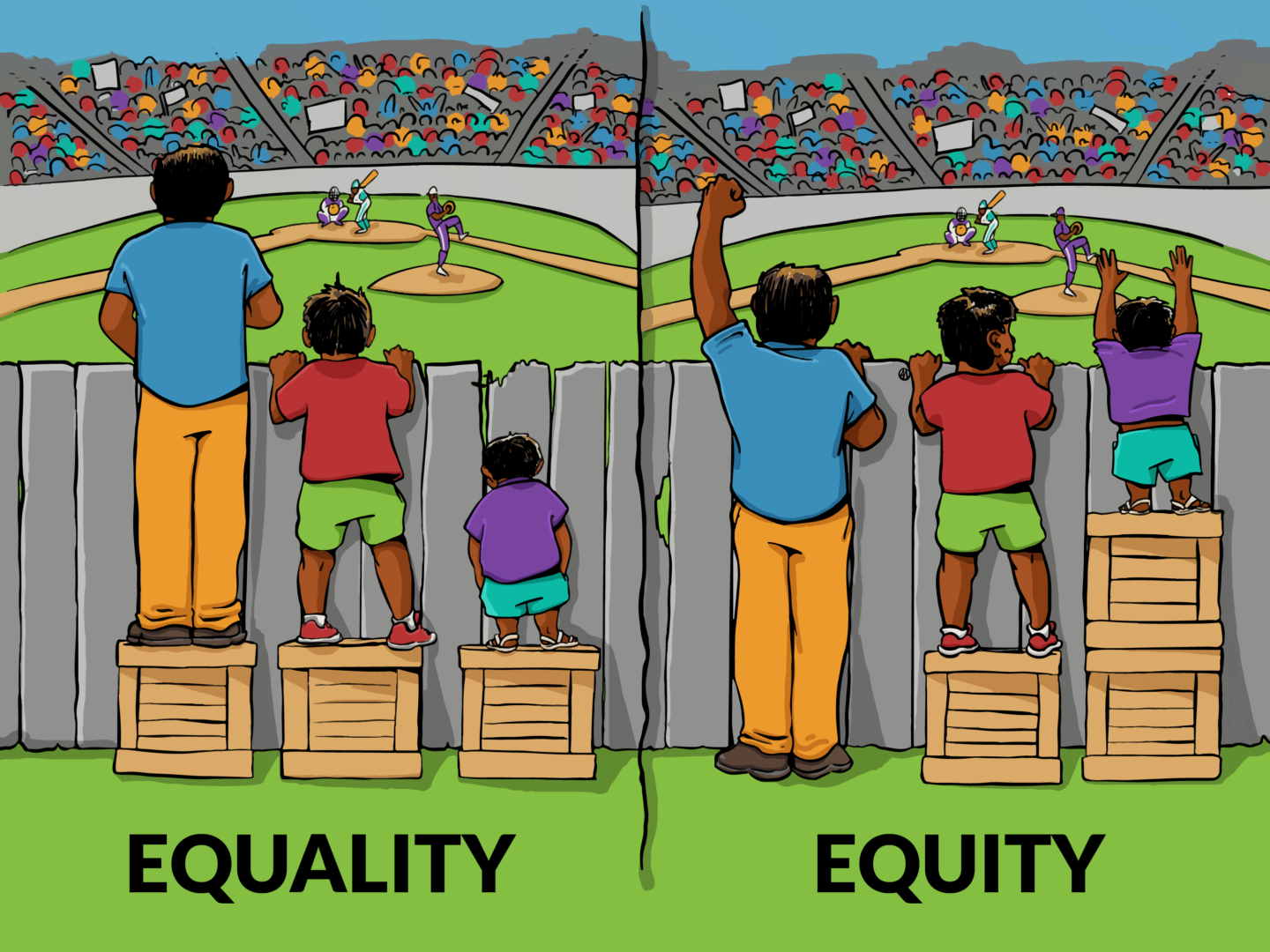
The oral-systemic connection during pregnancy also underscores a notion we have mentioned in all three parts of this series: integrated health care models are key to optimal outcomes. Expecting mothers have a lot do deal with, including a plethora of health care needs, from OB-GYN visits to primary care, birth counseling, and more. This takes time (and time off from work), which is hard to come by for many. We understand that adding oral health care into the mix can be easier said than done.
Integrated health care models, however, offer a way to make care during pregnancy easier on the expecting mother. Clinics and medical practices equipped to serve all the needs of a mother, from oral health care to OB-GYN services, could help ensure that pregnant women receive full-spectrum care to ensure as healthy a pregnancy as possible.
For more on the oral-systemic connection, be sure to read parts one and two of this series, and check out the resources below.
Sign up for NCOHC’s newsletter list to receive updates on stories like this one directly to your inbox.
NCOHC is a program of the Foundation for Health Leadership & Innovation. For more information and to stay up to date, subscribe to the NCOHC newsletter. If you are interested in becoming an NCOHC member, you can also fill out our membership form. It’s free!
Additional Sources for Information on the Oral-Systemic Connection
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3100856/
- https://www.ada.org/en/member-center/oral-health-topics/oral-systemic-health
- https://spectrum.diabetesjournals.org/content/24/4/187
- https://www.cdc.gov/diabetes/ndep/pdfs/ppod-guide-dental-professionals.pdf
- https://link.springer.com/article/10.1007%2Fs10995-014-1632-7
- https://www.ada.org/en/member-center/oral-health-topics/pregnancy
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5303728/
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3941365/
- https://www.nytimes.com/1996/10/09/us/gum-disease-in-pregnancy-linked-to-premature-low-weight-babies.html
- https://www.health.harvard.edu/heart-health/gum-disease-and-heart-disease-the-common-thread