This past November, the North Carolina Oral Health Collaborative welcomed two new staff members. Kelsey Ross Dew is NCOHC’s new program coordinator, and Brady Blackburn is the Collaborative’s content marketing specialist. As they pass the half-year mark, they sat down to answer a few questions about who they are and why they decided to join NCOHC.

Kelsey Ross Dew
Tell us a little about your background, where you are from, and your educational path.
I am from Severna Park, a town in Maryland situated right between Annapolis and Baltimore. Visiting family in North Carolina regularly, I became very familiar with the Wilmington area and was drawn to the university there.
I attended UNC-Wilmington, originally planning to go into nursing. I was exposed to so many fields and areas of study but just couldn’t choose. After looking at the courses closely, I decided on community health education for my undergraduate degree. That program at the time was transitioning to become the Public Health Program.
After graduating, East Carolina University offered a Master’s in Public Health program, so I decided to move from Wilmington to Greenville to pursue my MPH.
While working on my MPH, I worked as a research assistant for a childhood obesity prevention program. I was trained in research management, program management, evaluation and community engagement. I worked with that program for 2 years during my MPH and 2 years after graduating. Open to new opportunities at the time, I began to search for something different to focus on that would have a public health impact.
What professional accomplishment before coming to NCOHC are you most proud of?
I am most professionally proud of my master’s degree because it gave me time to build my skill set and learn.
What originally drew you to working in the oral health space?
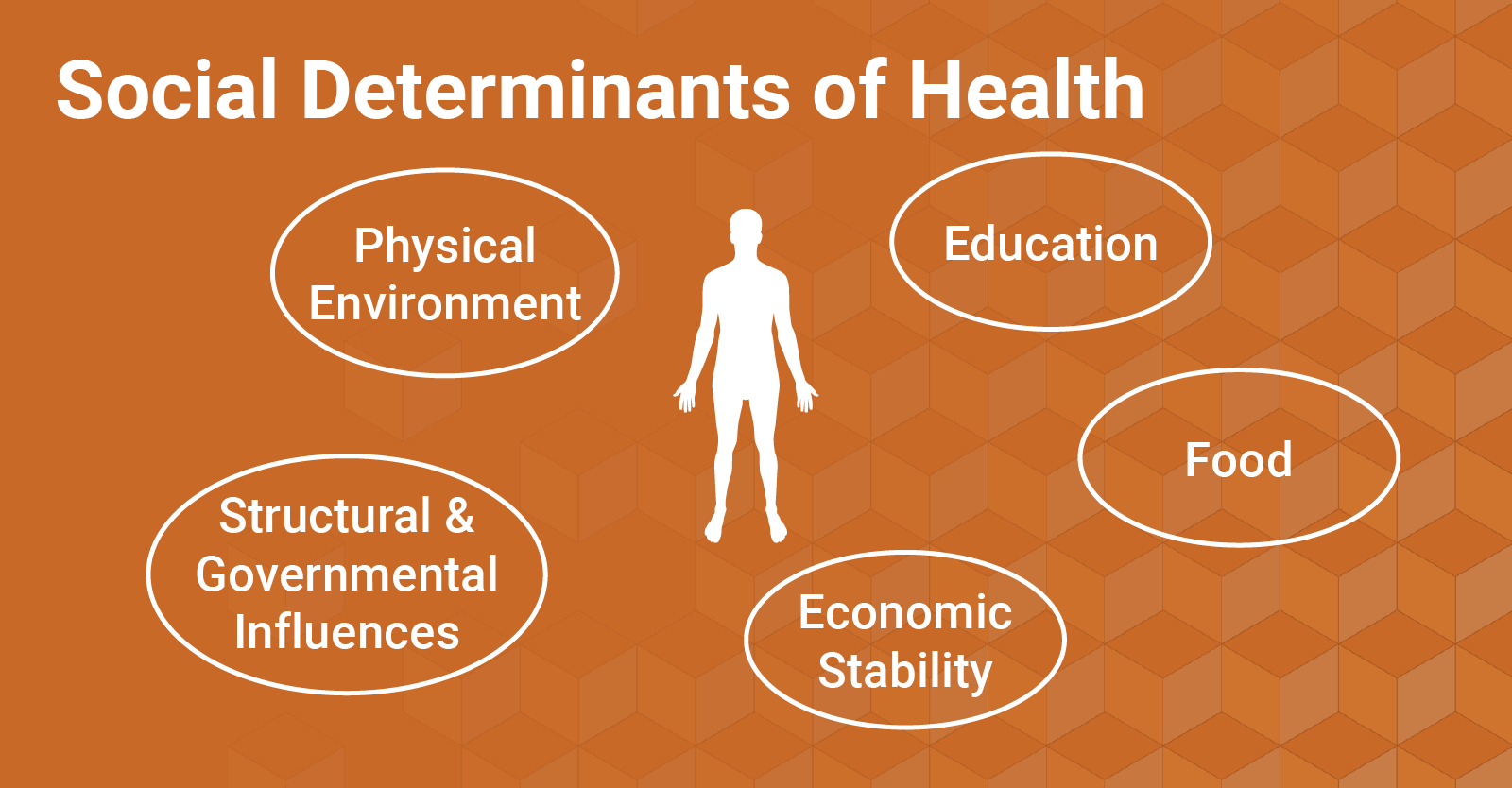
I saw the job posting for the program coordinator for NCOHC and started thinking about working in the oral health space. It quickly made me realize that I had not been exposed to the importance of oral health and public health dentistry previously. I wanted to transition to something different that would benefit the health of the whole person. Oral health seemed like an area that needed strong advocates and I wanted to be a part of that.
What has been the most rewarding part of your work with NCOHC thus far?
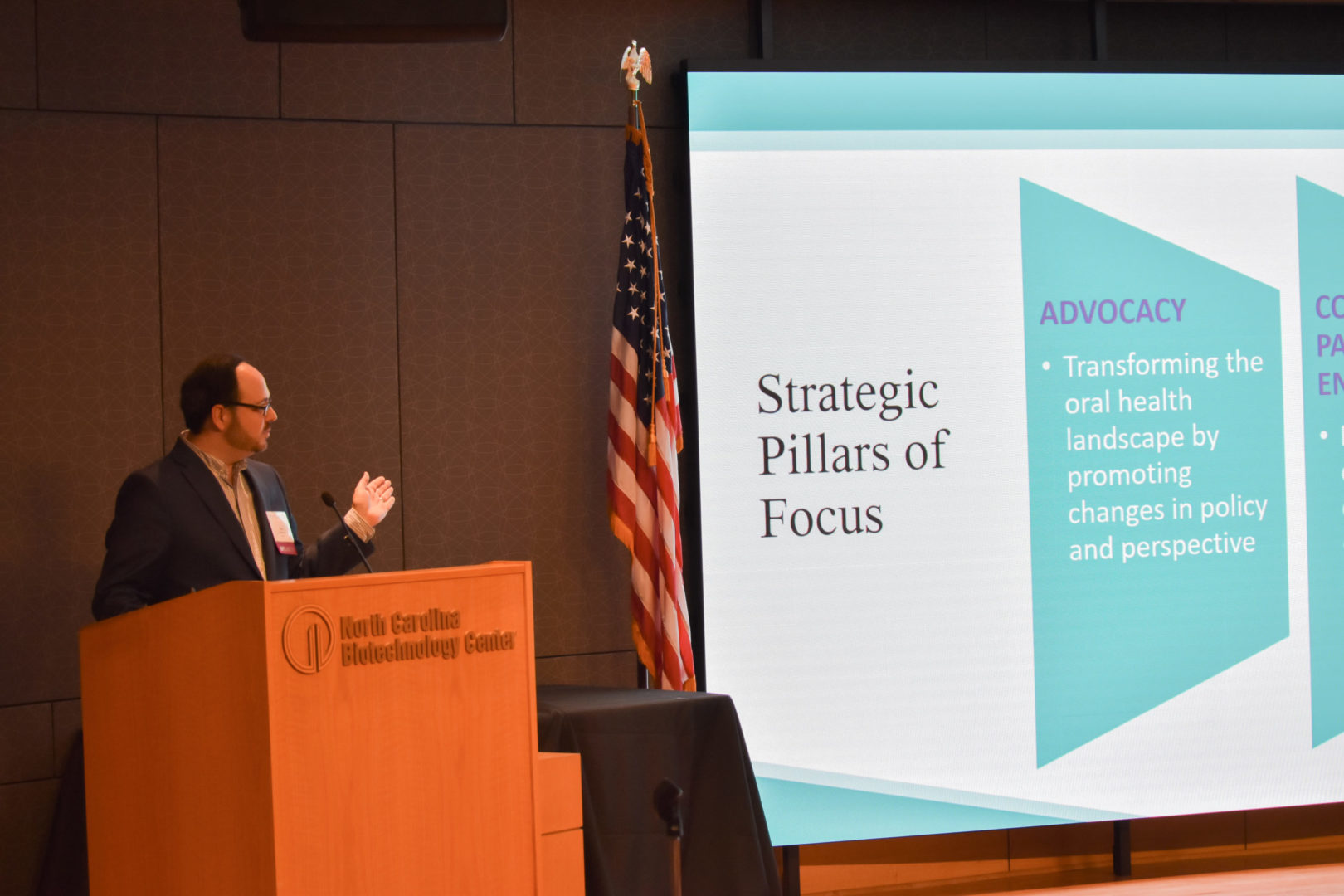
The most rewarding part of my work so far has been the different opportunities to be involved in policy change and engage with community. Policy changes have a large impact on increasing access and are a sustainable solution. In addition, I really think working directly with community and engaging them in the policymaking process can be helpful. It is rewarding to work towards solutions.
What are the biggest challenges that you see facing access and equity in oral health care in North Carolina?
I feel that there are systemic barriers to change through restrictive policy that limit access and equity in oral health care in this state. There are numerous policy solutions available that are evidence-based and would increase access and address oral health among the most vulnerable populations.
What do you enjoy doing when not working?
I enjoy spending time with my husband and dogs, whether that be at home or out around Raleigh. We enjoy games, sports, and traveling (when safe!). I like cooking as well!

What do you want our membership to know about you?
I want our membership to know that I am so grateful to be a part of this work and team. It takes a lot of committed individuals to make lasting changes. I also think prevention is key and we should focus efforts on increasing preventative solutions.

Brady Blackburn
Tell us a little about your background, where you are from, and your educational path.
I have lived in North Carolina for my entire life. I grew up in Asheville and went to college at UNC-Chapel Hill, where I was in the second graduating class of a dual-degree program that paired an undergraduate degree in environmental studies with a graduate degree in mass communication.
I worked in climate change communication for The Nature Conservancy during graduate school before moving back to Western North Carolina to run a 2018 state legislative campaign in Haywood, Jackson, and Swain Counties. We won the campaign, and I joined Joe Sam Queen as his legislative assistant for the first half of the 2019-2020 legislative session.
I have always been drawn to the nonprofit world, so after a while in the legislature, I began to turn my eyes toward new opportunities.
What professional accomplishment before coming to NCOHC are you most proud of?
Managing Joe Sam Queen’s legislative campaign was one of the more difficult things I have done. I am incredibly proud of our victory. In the seven-month stint between my graduation and the 2018 election, I grew in ways that I didn’t know were possible and I learned a lot from my first-hand experience with Representative Queen’s constituents in Haywood, Jackson, and Swain Counties.
What originally drew you to working in the oral health space?
In high school, I found myself on the wrong end of a golf club and lost my two front teeth. I would say that’s when I first became passionate about oral health care, and when I first understood how expensive more serious procedures can be.
Years later, in the North Carolina Legislature, our top priority was expanding access to affordable health care for underserved North Carolinians. I didn’t have a lot of experience in health and health policy going in, but I quickly learned just how stark the disparities our state are, and how vital policy is when it comes to increasing equity and access.
What has been the most rewarding part of your work with NCOHC thus far?
I’ve had several opportunities to interview people across North Carolina who work in oral health care or who have been impacted by a lack of access to that care. Hearing their stories has been incredibly moving, and it has really helped me understand the importance of the work we do.
What are the biggest challenges that you see facing access and equity in oral health care in North Carolina?
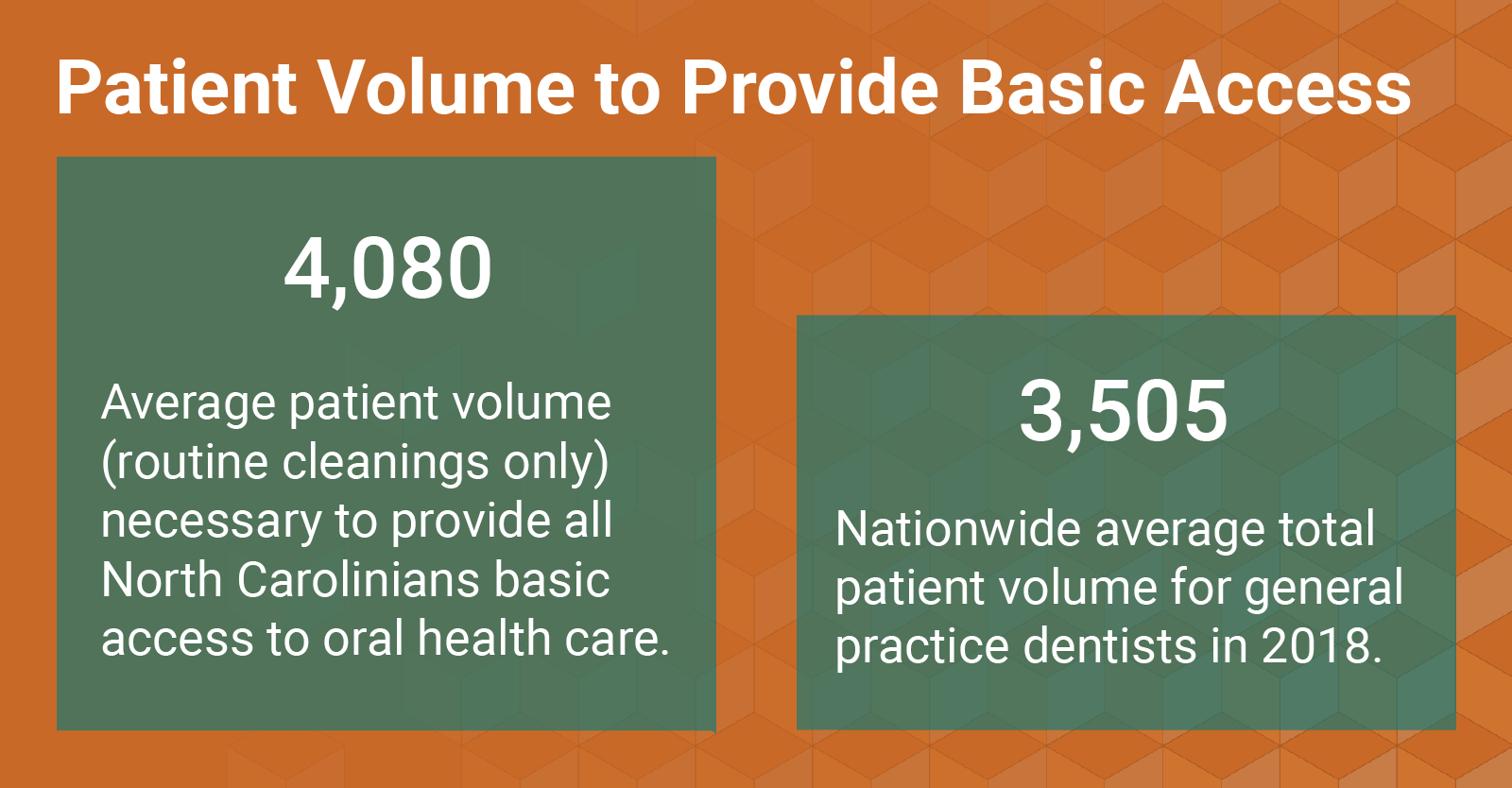
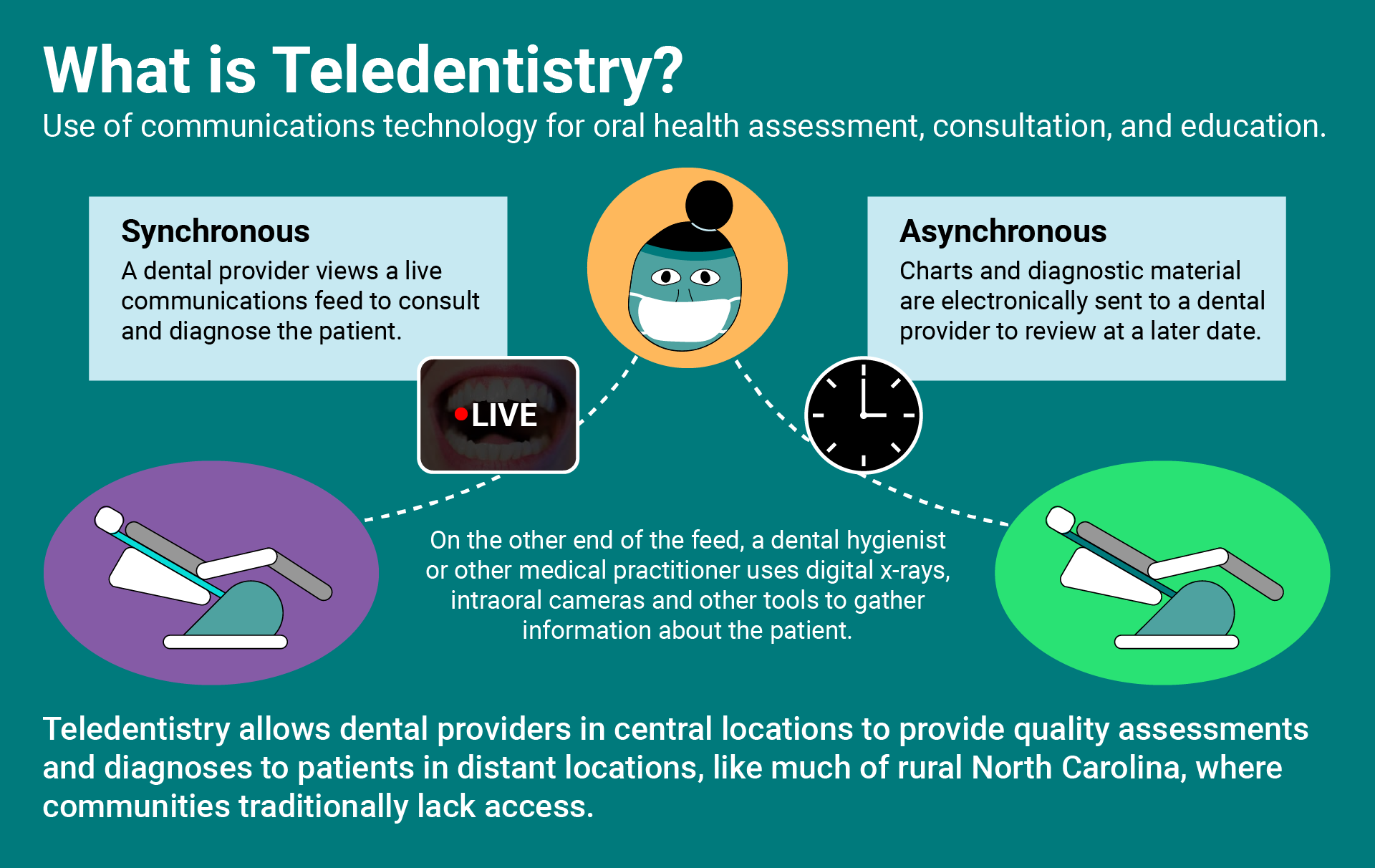
I think that there is a world in which oral health care is affordable for everyone. Preventive care is so much less expensive than restorative care, but unfortunately so many don’t have access or don’t know where to go before costly treatment is necessary. Creating an education infrastructure and building a system where care is accessible, no matter who you are or where in the state you live, seems to me to be the biggest step we could take towards achieving oral health care equity.
What do you enjoy doing when not working?
When I’m outside the office I love gardening, woodworking, and taking my dog on adventures. We love to go backpacking or just generally get outdoors.

What do you want our membership to know about you?
I want the membership to know that my (virtual) door is always open! I think that collaboration and storytelling are key to good communication, and there are so many amazing stories to tell about the people working hard to improve North Carolinians’ oral health.