Blog Posts
The Political Determinants of Oral Health
Daniel E. Dawes began his 2020 book, “The Political Determinants of Health,” with a story about a farmer looking for land to plant an orchard. He finds a plot of land split into three sections: one with rocky soil, one with poor soil, and one with rich soil. In the...
The Curb-Cut Effect in Oral Health
There are stories about “midnight raids” in the 1960s depicting disability rights advocates in Berkeley, CA, smashing and re-paving curbs so they would slope down to meet the street at intersections, allowing people in wheelchairs to cross. These stories aren’t...
How to Keep Your Gums Healthy, and Why It Matters
Teeth aren’t the only things in your mouth that need to be cared for. From your gums to your tongue, molars to canines, everything in your mouth needs proper care to stay healthy.
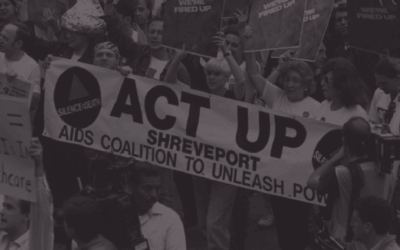
An Oral (Health) History of the HIV Epidemic
“It just kept happening, over and over and over again. Patients of record, patients I’d known for years. Either they come in complaining about something or I see something. All of the classic oral manifestations of HIV disease, there they were.” Dr. Lewis Lampiris is...
The Medicaid Access Gap for Children in North Carolina
It’s no secret that there is an oral health care access gap for North Carolinians with Medicaid insurance. It’s practically a rule of thumb that if you are born poor, you will have less access to health care services (medical and dental), and in turn will likely end...
How To Become a Dental Hygienist in North Carolina
Dental Hygiene Programs North Carolina has fourteen Commission on Dental Accreditation (CODA) approved dental hygiene programs. These include 13 Associate of Applied Science degree programs at community colleges throughout the state and one baccalaureate...
Social Justice, Dentistry, and Forensic Testimony in the Courtroom
On April 8, 2002, Ray Krone was released from prison after serving 10 years for a murder he did not commit. A decade earlier, a woman’s body was found at the bar Krone frequented. Officers identified Krone as a person of interest, and they took a Styrofoam impression...