Last week we had the opportunity to take an in-depth look at teledentistry at Oral Health Day Part 2. Three North Carolina dental directors and a panel of national experts took questions and presented to a crowd so large that we had to upgrade our Zoom subscription mid-event!
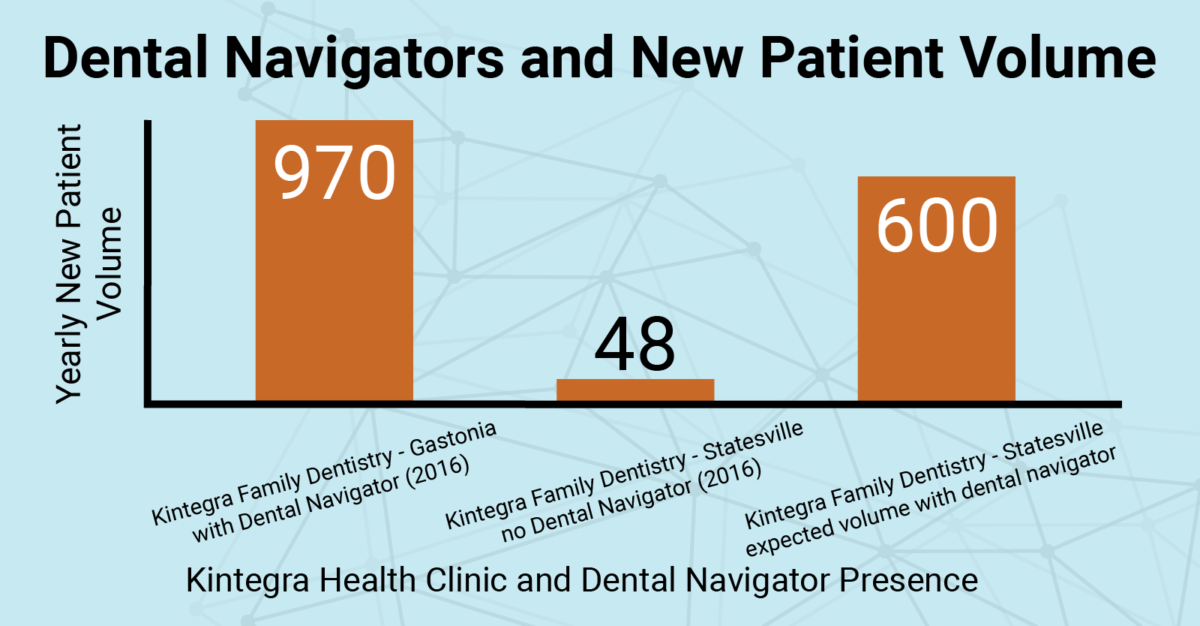
The dental directors at Kintegra Health, Piedmont Health, and Greene County Health Care (GCHC) kicked off the day, talking about the many ways their Federally Qualified Health Centers (FQHCs) use teledentistry to improve patient care. All three directors took questions from the audience.
“Know where you’re going and have a roadmap,” said Dr. Mattison-Chalwe, answering a question about the planning process to successfully begin using teledentistry technology in a practice.
The dental directors answered questions and discussed everything from the planning process, to tips and tricks, to getting diagnostic-quality patient information, and the ways that new technology has increased clinic efficiency.
“We got a lot closer to medical,” said Dr. Doherty, referring to the relationship GCHC’s dental facility was able to make with their medical counterparts as they implemented teledentistry protocols. “It is very easy for a provider to give us a call — a medical provider, and we just jump right in on the call and get those patients seen very quickly.”
Watch Drs. Donigan, Mattison-Chalwe, and Doherty in three live teledentistry demonstrations.
After the dental directors spoke, three nationally recognized teledentistry experts took the virtual stage. Dr. Paul Glassman, the “father of teledentistry” and professor and associate dean for research and community engagement at California Northstate University College of Dental Medicine, spoke about the process of actually “doing teledentistry,” and the future of remote care.
“This is really based on calibration and communication,” said Dr. Glassman. “It’s based on the idea that you’re going to trust the hygienist who is in the community.”
Dr. Scott Howell, assistant professor and director of teledentistry at the A.T. Still University Arizona School of Dentistry & Oral Health, walked the audience through several examples of the various ways he uses teledentistry in his clinical practice.
Dr. Howell mirrored Dr. Glassman, saying that collaboration and communication is key to successfully using teledentistry technology.
“The field team must be calibrated,” said Dr. Howell. “There has got to be trust. Trust between dentist and hygienist; the dentist has to trust the technology. And as I tell my students, this is not something that you develop overnight. It is something that takes time to develop.”
Brant Herman, CEO of MouthWatch — a provider of teledentistry software and equipment — spoke about the actual technology necessary to practice via teledentistry. He also covered common misconceptions about what it takes to incorporate remote care in a clinical setting.
One of the bigger misunderstandings highlighted by Herman is the idea that there is only one way to do teledentistry.
“It’s really just the tool. You’re just using the technology as the tool,” said Herman. “You’re facilitating the other approaches to care coordination, care delivery, through this technology. It can be all of these different services that really just use teledentistry as the backbone to connect patients, providers, and care.”
MouthWatch, LLC, was generous enough to donate four intraoral cameras for the event, which NCOHC raffled off live.
NCOHC has worked collaboratively alongside diverse stakeholders in jointly drafting teledentistry legislation, which is slated to be introduced during the 2021-2022 legislative session. This bill will work to improve providers’ ability to incorporate teledentistry technology in their practices, and will ensure that quality oral health services, aided by teledentistry, are delivered equitably throughout North Carolina.
Stay tuned as we move forward. We encourage and welcome all voices at the table, so please consider signing up to receive our newsletter, and help us create a more equitable oral health landscape in our state.
NCOHC is a program of the Foundation for Health Leadership & Innovation. For more information and to stay up to date, subscribe to the NCOHC newsletter. If you are interested in becoming an NCOHC member, you can also fill out our membership form. It’s free!