In North Carolina, nearly 90 percent of the population is serviced by fluoridated water. This is not the case in Western North Carolina, where rates are estimated to be much lower. Limited access to fluoride means detrimental consequences for many people in the western region of the state, where people are more likely to suffer from tooth decay and other oral health complications. Without sufficient fluoride access, people are more vulnerable to these conditions.
Along with the lack of regular access to fluoridated water, there are other drivers that lead to the negative oral health conditions that are so prevalent in WNC. Consuming large amounts of sugar can be a major component for accelerating tooth decay. The acids in sugar damage the enamel on the outer layer of the teeth, leaving them more vulnerable to bacteria, which leads to cavities and gum disease.

Fluoride, however, plays a significant role in overall oral health outcomes in a given area. Fortunately, even in places like WNC where access to fluoridated tap water is not as widespread, there are other means of accessing the preventive mineral.
Regular brushing is important to keep bacteria under control. There are many fluoridated options for toothpaste, which are more effective in protecting teeth than non-fluoridated options.
For children in North Carolina, physicians in primary care medical offices can apply fluoride varnish that sticks to hard-to-reach areas of the teeth. Dentists can also paint on sealants for patients to help shield teeth from bacteria and prevent cavities. Fortunately, the public health division in North Carolina has also trained dental hygienists to be able to provide some of these preventive services.
Click here to see how Kintegra Health is improving WNC children’s oral health with its Dental Access Program, sending hygienists into schools to provide preventive care, including dental sealants.
We recently spoke in a virtual interview with University of North Carolina Distinguished Professor Gary Slade about the consequences of inadequate access to fluoride. Dr. Slade, who has worked in the Division of Pediatric and Public Health at the Adams School of Dentistry since 1994, works largely on epidemiological research that focuses on oral health and dental diseases in populations.
Dr. Slade explained that data show that children with access to fluoridated water have 30 percent fewer cavities in their baby teeth. As adolescents, they have 12 percent fewer cavities. Fluoride provides clear preventive oral health benefits, which makes the low rates of fluoridated water in WNC especially alarming.
“Because fluoridation rates in Western North Carolina do not count well water or sources that are not from tap water, the numbers we have from data with regard to tooth decay and other oral health conditions are probably worse than they appear,” Dr. Slade said.
As is the case with many small towns in Western NC, cost plays an important role when it comes to providing fluoride for communities. After being accustomed to living without fluoridated water, introducing it is not always seen as a priority. Engineering obstacles in some of these rural areas may also be a deal-breaker for many.
So, what is being done to enact change?
The first and most important step is advocacy. Whether it be a dentist, engineer, public health agency, or parent who speaks up first, change must begin at a local level. Dr. Slade explained that change is not guaranteed to happen just because it seems like the right thing to do. An effort like increasing access to fluoridated water begins with someone championing the cause.
Dr. Slade also spoke about important research he will be conducting in 2021 in Kinston, North Carolina, on the preventive effects of fluoridated bottled water. It is estimated that 115 million Americans do not have access to fluoride in their drinking water at home. That is roughly one-third of the American population, a number that Dr. Slade says will not significantly change in the near future.

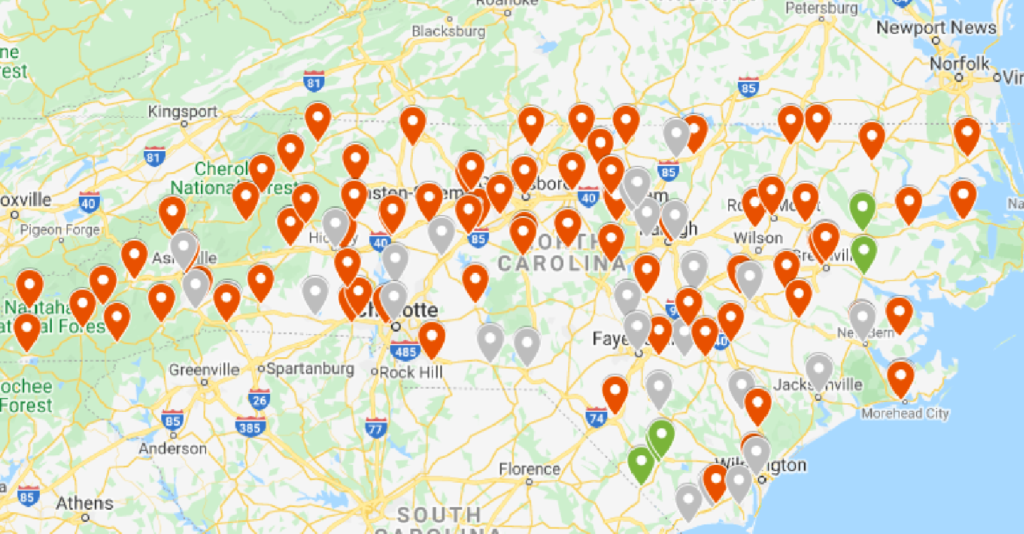
Kinston resides in Lenoir County, located in eastern North Carolina. Dr. Slade described it as a prime example of a city that will not likely introduce fluoride into the public water system anytime soon.
Traditionally, dentists and oral health professionals have discouraged people from drinking bottled water due to the lack of fluoride, since most companies do not include it. However, with the rise in popularity of bottled water, Dr. Slade is taking a different approach. Rather than encouraging people to avoid bottled water, the upward trend in popularity would suggest that promoting the inclusion of fluoride in bottled water may be the best approach to improving access to better oral health.
There are many reasons why fluoride access is limited in some parts of the country, but one of them may be the criticism it receives. Dr. Slade suggested that some skepticism may be due to the fact that there has not been a randomized controlled trial of fluoridated water. His study in Kinston will be the first.
The study will include 200 participants, divided into two groups. One group will be given fluoridated bottled water, and the other will be given unfluoridated bottled water. After a period of three and a half years, each participant will receive a dental examination. Because of the true randomized design, no participant or researcher will know who had fluoridated water and who had unfluoridated water until the study is complete.
Dr. Slade expects the resulting data to speak for itself.
Today, it has become increasingly more difficult to implement public fluoridated water systems. There is a significant amount of advocacy from individuals and interest groups on both sides of the issue.
Dr. Slade said that with lower levels of health literacy, it is also more likely that misinformation will stick in people’s minds. Changing that starts with advocacy and education in schools at an early age. There are a lot of questions that surround the topic of fluoride in the United States, but more importantly, there are a lot of answers. Fluoridated water as we know today, provides the easiest and most efficient form of preventive care for lifelong oral health benefits.
Want to get involved and elevate your voice? From fluoridated water and teledentistry to the rising cost of health care, NC4Change is a platform for a diverse, inclusive group of oral health practitioners, public health professionals, community members, and other stakeholders who share a common goal: increasing equity and access in oral health care.