The North Carolina Oral Health Collaborative (NCOHC) released its first policy brief earlier this year, outlining a broad array of policy changes that, if enacted, would improve access and equity in oral health care for all North Carolinians.
Read the full policy brief here
Improving payment models can have a considerable impact on the care people receive, increasing efficiency and improving health outcomes. Payment reform refers to health care models that use reimbursement from insurers to providers to promote greater value for patients, purchasers, payers, and providers.
This third and final deep dive into NCOHC’s policy brief will focus on the payment reform section, elaborating on changes that can be made to make oral health care more efficient and affordable.
Teledentistry and Parity of Payment
Teledentistry has proven to be an effective means of connecting patients with their providers, especially during the COVID-19 pandemic. While remote care has proven to be invaluable in ensuring patient and provider safety, it is also a useful tool to increase equity in care, even in a post-pandemic world.
Unfortunately, some insurance plans do not reimburse for teledental services similarly to how they pay for in-person care.
Providers, especially in safety-net settings with thin profit margins, already frequently use teledentistry, sometimes without reimbursement. Safety-net providers will continue to use teledentistry to provide patients with essential care, and it is important that payment systems support this innovation in care delivery through equitable payment schedules.
Data suggest that patients receive the same quality of care via teledentistry as they do in person. For this reason, NCOHC recommends parity of payment across insurers.
Silver Diamine Fluoride
During the pandemic, there has been an increased focus on preventive care that reduces the amount of close-contact dental visits. One valuable resource in the realm of non-aerosolizing cavity management is the use of Silver Diamine Fluoride (SDF).
Aerosolizing refers to anything that can convert material into a fine spray that can be suspended in the air. Some dental procedures run the risk of aerosolizing the COVID-19 virus, leading providers to look to other, non-aerosolizing options.
When applied directly to a cavity, SDF can have a significant impact on reducing future urgent or emergent dental needs. As an efficient and cost-effective tool that doesn’t risk aerosolizing anything in the mouth, SDF is an ideal treatment to use during the ongoing pandemic.
Prior to COVID-19, payment for SDF varied widely. While NC Medicaid covered SDF, reimbursement was limited for patients five years old and younger. In vulnerable populations, however, many children may not even see a dentist before that age.
While NCOHC commends NC Medicaid for lifting all age restrictions for SDF reimbursement in response to COVID-19, it is important that these payment policies continue post-pandemic.
NCOHC recommends that NC Medicaid reimburse SDF placement for patients of any age. This will allow for more equitable access to this evidence-based treatment for both vulnerable children and adults.
NCOHC also recommends that the private payer sector incentivize SDF as a viable treatment through enhanced reimbursement policies.
Interim Therapeutic Restoration
Other viable options for non-surgical treatment of dental caries include Interim Therapeutic Restorations (ITRs). ITRs are non-permanent restorations placed on teeth to prevent cavities from progressing. Even though they are temporary, ITRs are effective reducing the negative impacts of caries until more permanent treatments can be administered.
Keeping in mind that many children rely on school-based care, this method of addressing tooth decay is particularly important because it could be delivered by hygienists, often at a lower cost. ITRs can dramatically help offset emergent needs in the immediate future. However, in North Carolina, this would be contingent on revision of delegated duties for dental hygienists.
Although many private payers currently reimburse for ITRs, a payment analysis should be done to ensure that they are incentivized as effective treatments through adequate payment models. Post COVID-19, NCOHC encourages NC Medicaid to also reimburse for ITRs.
Value-Based Oral Health Care Payment
As oral health care shifts toward a more value-based approach, focused on improving patient outcomes and lowering costs, it is necessary to think holistically about both the quality of care being delivered and how the care is delivered.
Care coordination management, addressing appointment compliance, motivational interviewing, and patient education to improve oral health literacy are services that should be covered by public and private payer sources to enhance patient-centered care.
These can be useful tools in helping people navigate treatment plans, coordinate transportation, and generally feel more comfortable engaging in social service support. All of these efforts can impact successful delivery of quality oral health care and improvement of patient outcomes.
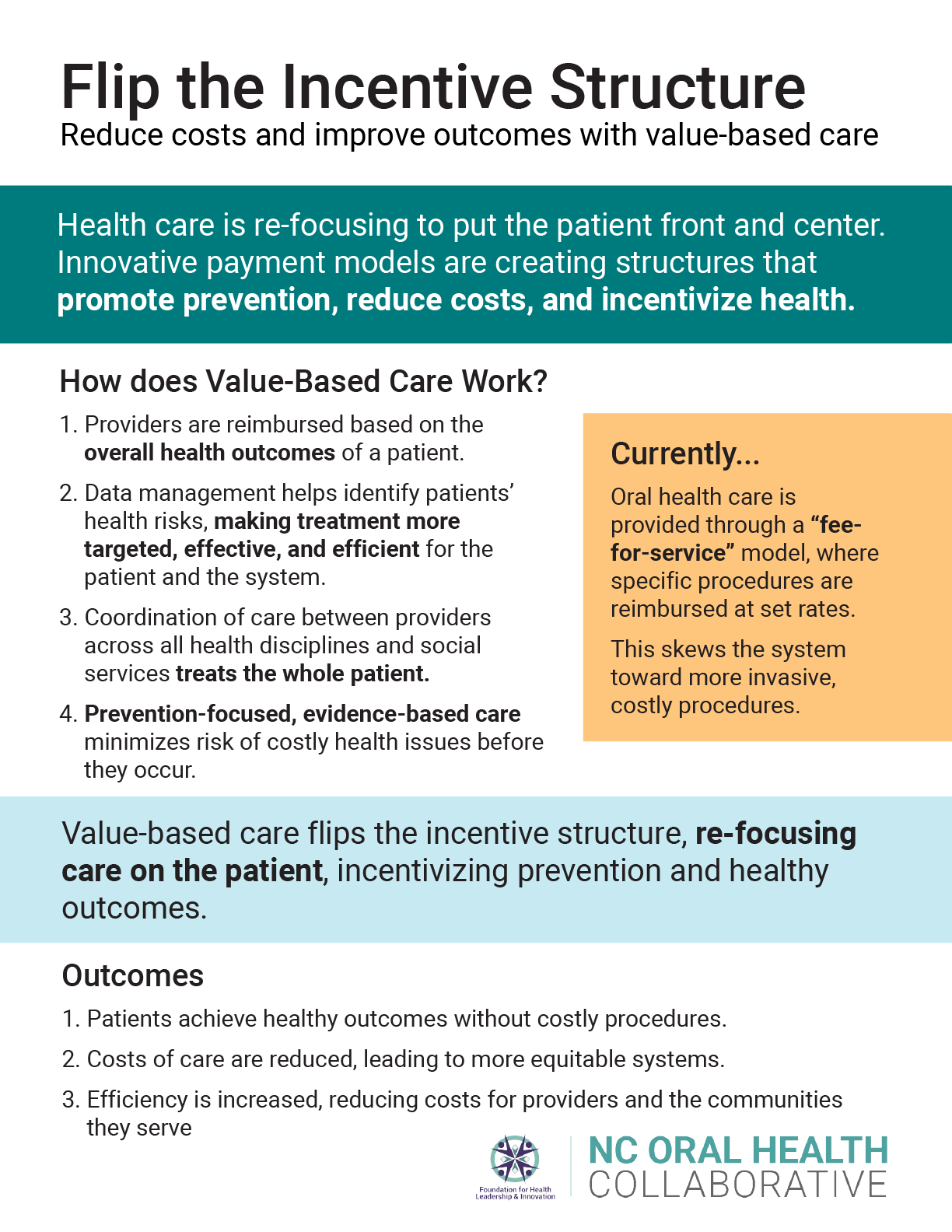
Patient-centered care also means a patient-centered approach to financing.
When it comes to oral health management, emphasis should be placed on prevention. For vulnerable populations, it is often unknown when patients will be able to return for care. Bundling payment for services such as comprehensive oral health evaluations, prophylaxis for adults and children, topical application of fluoride and varnish, and sealants would incentivize providers to cover necessary services in a single visit.
NCOHC also recommends bundling nutritional counseling, tobacco counseling, and oral hygiene instruction as adjunctive non-paid services.
Payment reform and public policy must work in conjunction with one another to achieve long-lasting results. More often, payment reform drives changes in public policy. This means that Medicaid and private payers play a particularly important role in facilitation innovation in public health. As we begin to find new measures of success in value-based care, implementing these necessary changes will help improve peoples’ health and transform the oral health landscape.
NCOHC is a program of the Foundation for Health Leadership & Innovation. For more information and to stay up to date, subscribe to the NCOHC newsletter. If you are interested in becoming an NCOHC member, you can also fill out our membership form. It’s free!