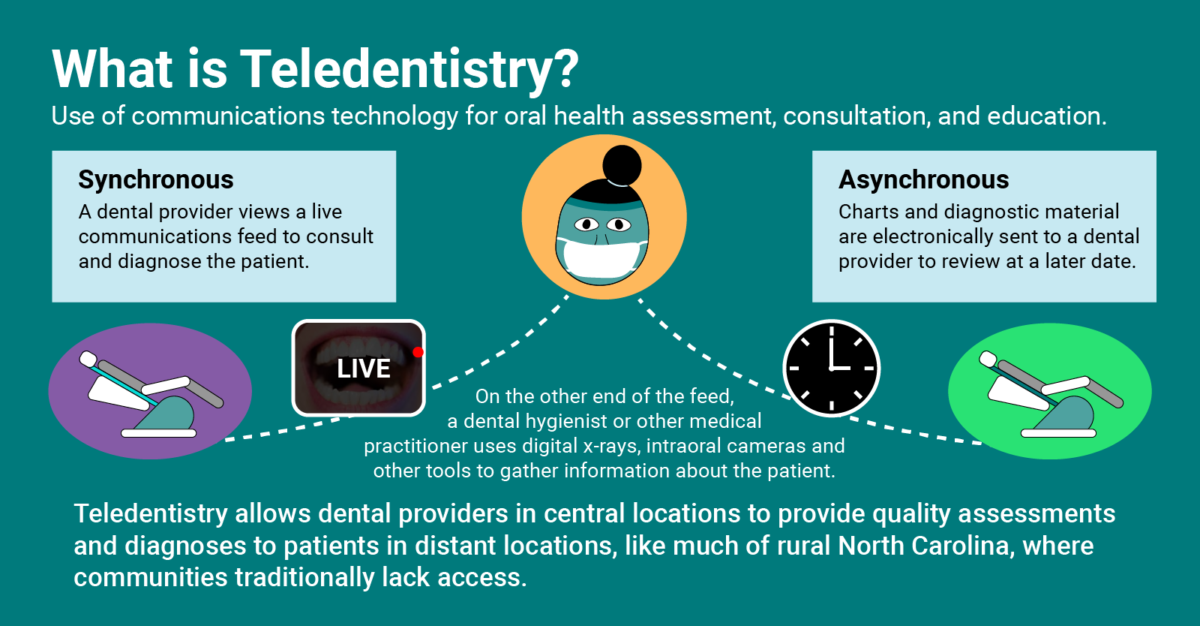
The COVID-19 pandemic has made it very clear that telemedicine is a necessary tool in most healthcare fields. Teledentistry in particular has been an effective means of connecting patients with oral health care providers while prioritizing patient and provider safety. However, beyond the scope of health care during a pandemic, teledentistry has invaluable benefits that will continue to improve equity and access in care, even post-COVID-19.
That’s why improving the legal framework around teledentistry is one of NCOHC’s top priorities in 2021.
Why does policy change need to happen for teledentistry to be used?
Any dental provider anywhere in North Carolina can use teledentistry to some extent today. However, teledentistry is not well-defined in North Carolina’s Dental Practice Act—which makes sense, as remote care technologies are fairly recent innovations.
Fortunately, the North Carolina Division of Health Benefits (NC Medicaid) did enact temporary provisions allowing providers to bill for teledental services while the COVID-19 pandemic continues to require heightened safety precautions. Private payers in NC have also embraced teledentistry by incentivizing its use during COVID-19. NCOHC believes that these provisions should be made permanent.
Why do we need teledentistry post-COVID-19?
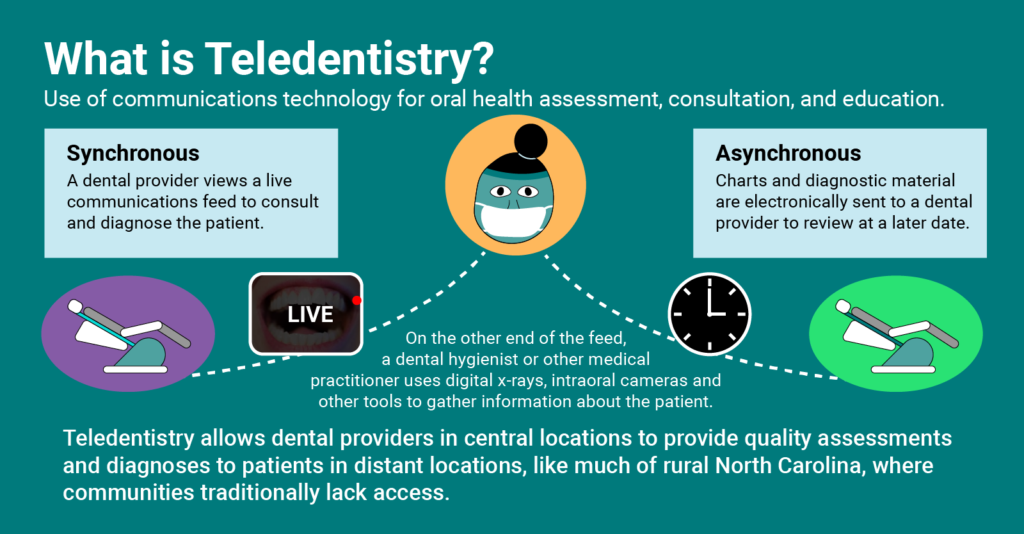
Teledentistry is an important means by which to increase access and equity in oral health care. There are counties in North Carolina without any practicing dentists. Expanding the use of teledentistry and permanently adopting appropriate payment models would allow many North Carolinians, especially in rural areas, to access care they might otherwise not receive.
There are several social determinants of health that affect a person’s ability to access reliable health care. Some of the biggest include lack of access to reliable transportation, the inability to take time off work and, for parents, difficulty finding someone to take care of their children while they are away.

Teledentistry can be used to help overcome some of these barriers. Obviously, dentists cannot fill a cavity remotely and a hygienist won’t be cleaning teeth remotely. Nevertheless, streamlining the process can significantly ease the burden on patients short on time, transportation, and more.
Take for example a patient who goes into the office for a routine exam and cleaning appointment and is found to have a cavity. Often, the filling is scheduled as a follow-up appointment. If basic screening is conducted remotely, the required two trips to the office, two periods of time off work, two babysitters, and so forth, could possibly be cut in half.
On the flip side, follow-up appointments to check in with patients who recently had work done can be conducted remotely, again reducing the burden on those seeking care.
For more information on teledentistry, visit our accompanying blog post, “Envisioning Teledentistry in North Carolina.”
So, what’s next?
Permanently adopting teledentistry payment models would reduce obstacles for dentists who want to offer remote care options and provide greater efficiency in care delivery.
Providers — especially those in safety-net clinics with thin profit margins — already frequently use teledentistry, often without reimbursement. Safety-net providers will continue to use teledentistry to provide patients with essential care, and it is important that payment systems support this innovation in care delivery through equitable payment schedules.
Stay tuned as NCOHC works during the 2021 legislative session to ensure teledentistry legislation is passed. Head over to NC4Change and help us take steps forward for positive change today.
NCOHC is a program of the Foundation for Health Leadership & Innovation. For more information and to stay up to date, subscribe to the NCOHC newsletter. If you are interested in becoming an NCOHC member, you can also fill out our membership form. It’s free!