Haven’t had time to read the new HPI Report analyzing access for children and adults with Medicaid/CHIP insurance in North Carolina yet? We’ve got you covered.
Earlier this year, the American Dental Association Health Policy Institute, in collaboration with the North Carolina Dental Society and the North Carolina Department of Health and Human Services, published an analysis of access to oral health care for North Carolinians with Medicaid/CHIP Insurance.
To provide context as we continue to break down the report and discuss next steps to create a more equitable, accessible North Carolina, we put together a brief summary of the report’s highlights.
Key findings from HPI’s analysis include:
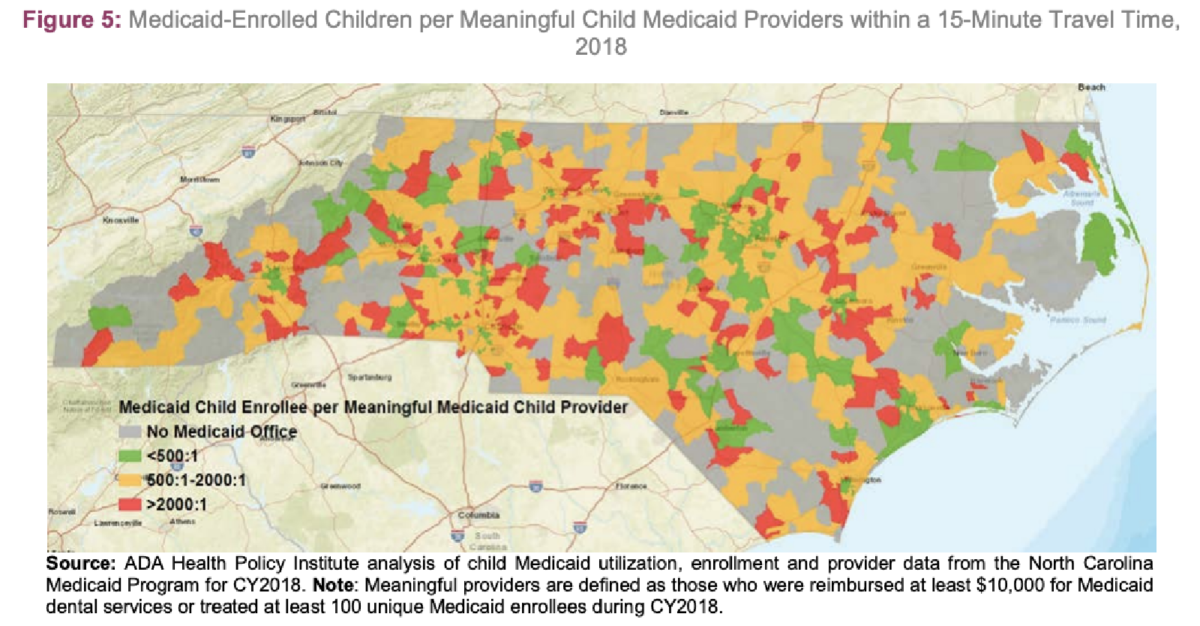
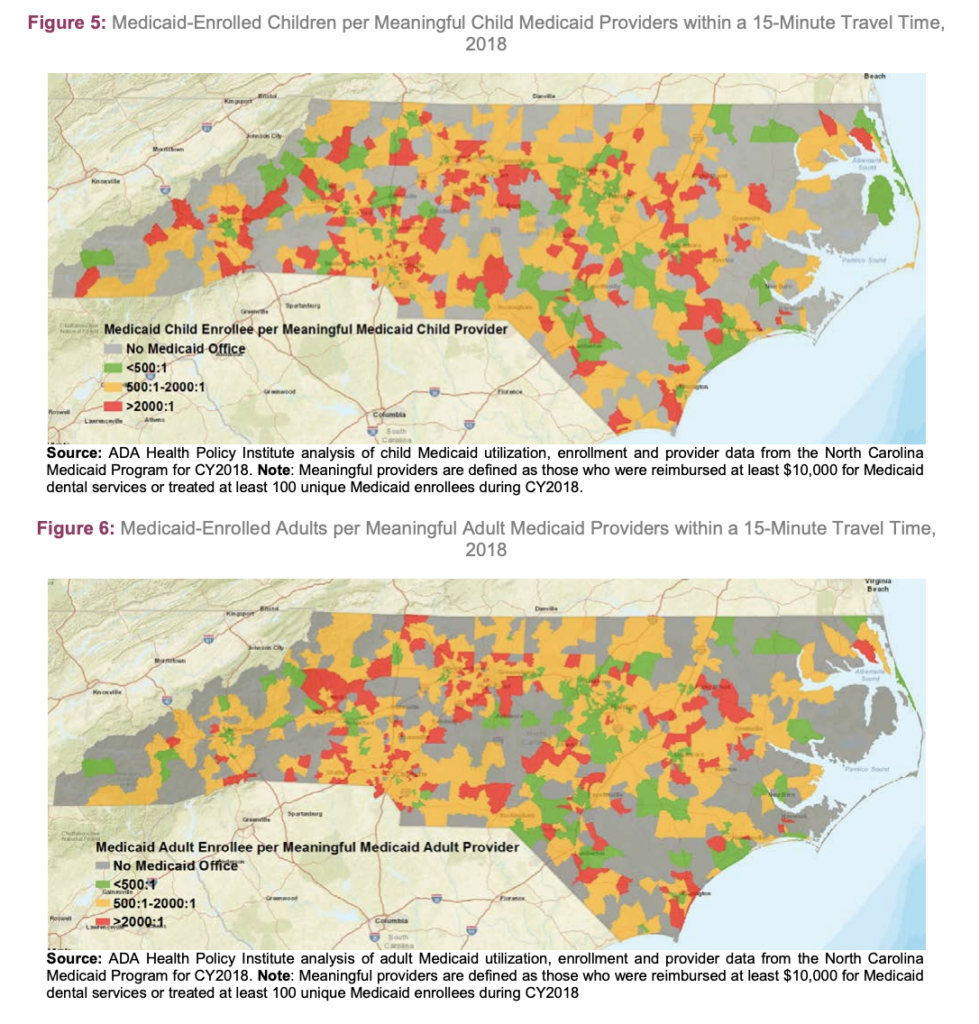
- Supply of “meaningful” providers—meaning providers who meet a benchmark of $10,000 in Medicaid claims each year—varies geographically for both children and adults.
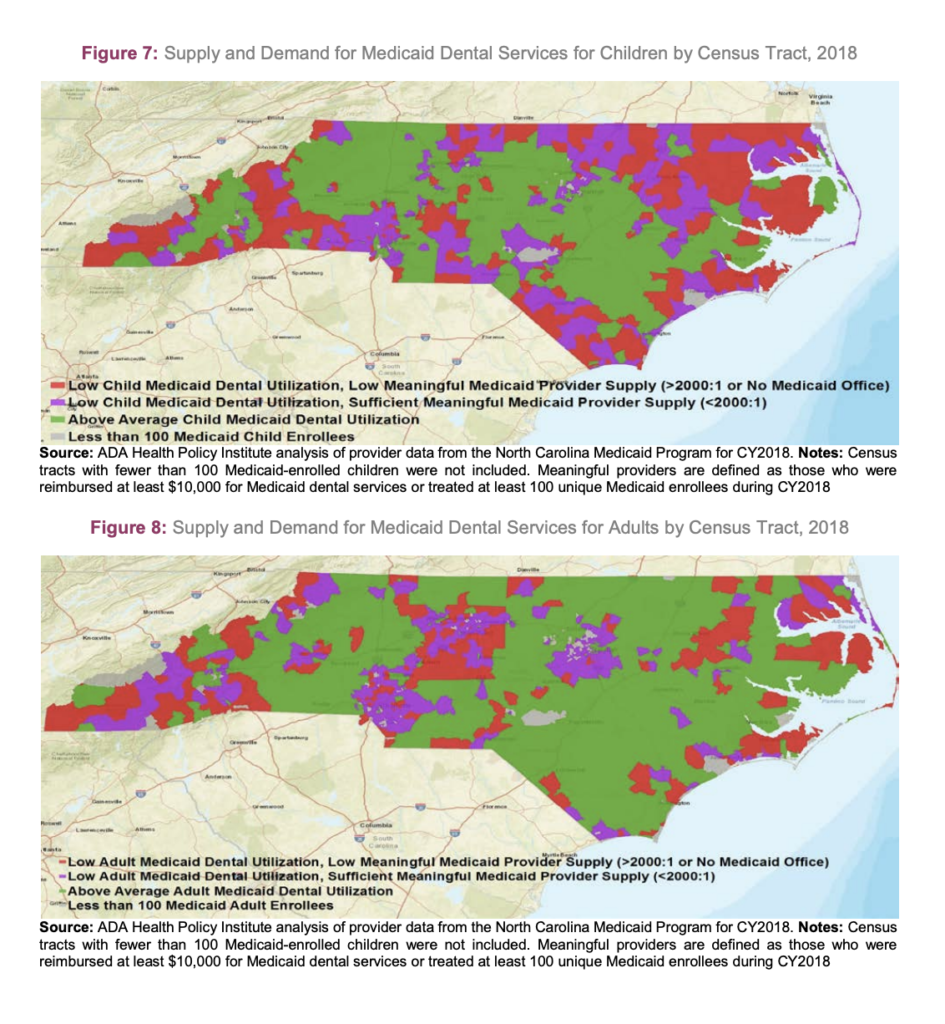
- While overall utilization among children is above the national average, with 58.9 North Carolinian children seeing a dentist within the past year versus 51.7 percent nationwide, there are also areas where utilization falls below 25 percent.
- Dental care utilization among Medicaid-insured adults is low, at 18.7 percent statewide, versus 23.2 percent nationwide.
- Medicaid-insured individuals are less likely to secure appointments compared to their privately insured counterparts.
Dr. Mark Casey, dental officer for the North Carolina Division of Health Benefits (NC Medicaid), penned an introduction to the report, tracing a history of innovation from the groundbreaking 1998 North Carolina Institute of Medicine “Task Force on Dental Access,” to a landmark lawsuit requiring NC Medicaid to raise reimbursement rates, and to the creation of “Into the Mouths of Babes”.
“NC Medicaid and its partner, the North Carolina Dental Society, agree that there is much work left to do to fulfill the promise of better oral health for the disadvantaged in our state,” wrote Casey. “However, it is also important to take note of the progress that has been made over the last 20 years from a time when the vast majority of publicly insured children were not receiving an annual dental visit.”
Casey also recently sat down with NCOHC for an interview about the HPI Report and his takeaways, which you can read here.
The HPI Report authors found that 90 percent of Medicaid-insured children live within 15 minutes of a participating dentist. It is important to note that this figure includes the entire pool of participating providers, not just “meaningful providers.”
When you filter for meaningful providers and break the data down geographically, access gaps begin to emerge.
The HPI Report authors outlined two important factors that contribute to North Carolina’s access gaps: the supply of dentists and the demand for dental services.
In the images above, red areas signify more than 2,000 Medicaid/CHIP-insured patients per meaningful provider. The grey areas, which are especially significant in the western and eastern parts of the state, lack a Medicaid office altogether.
When comparing supply versus demand, a clearer picture emerges, highlighting Northeastern and Western North Carolina as the two regions with the most pressing access disparities.
Looking forward, there are both good and bad signs for North Carolina…and there is a lot of work that can be done to increase access and equity in care.
On average, Medicaid/CHIP-insured patients have a more difficult time securing appointments compared to their privately insured counterparts. What work can be done to end this disparity?
HPI projected a net increase in practicing dentists in North Carolina in the coming years. Can North Carolina provide adequate incentives to encourage new providers to practice in underserved, rural areas?
Be sure to stay tuned for NCOHC’s perspective on the findings in the HPI Report and the collaborative’s suggestions for next steps to increase access and equity in oral health care! We will publish a full analysis soon. In the meantime, here are a few of our immediate takeaways:
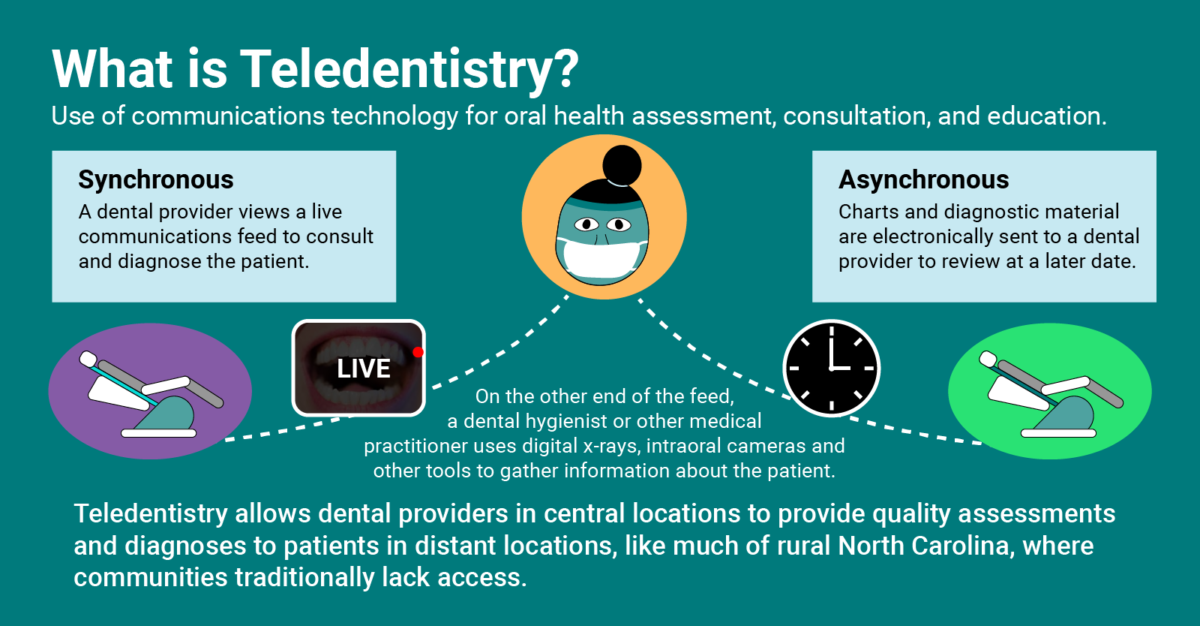
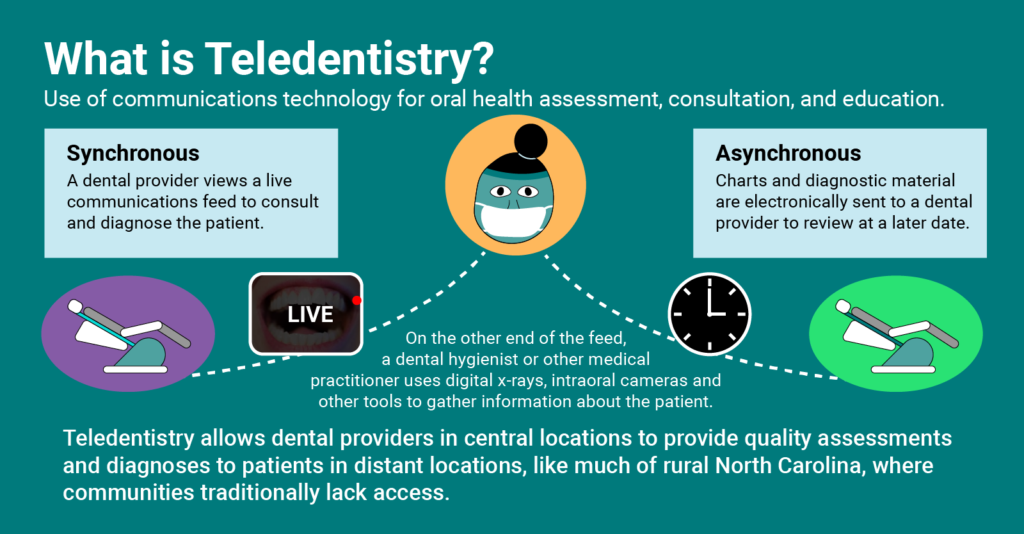
- In rural NC, innovative approaches to practicing dentistry — such as teledentistry and school-based care— can significantly improve access to those with Medicaid/CHIP insurance.
- We need North Carolina stakeholders to work together and find innovative ways to incentivize newly graduated dentists to serve patients in underserved regions.
- We are excited to work with stakeholders, both in private practice and public health, to find ways to increase the number of dentists serving Medicaid/CHIP patients, and similarly, to increase the number of patients participating dentists serve each year.
What changes do you think will help North Carolinians? Get involved by heading over to NC4Change and signing up for a focus group today!
NCOHC is a program of the Foundation for Health Leadership & Innovation. For more information and to stay up to date, subscribe to the NCOHC newsletter. If you are interested in becoming an NCOHC member, you can also fill out our membership form. It’s free!












 العربية
العربية 简体中文
简体中文 English
English Filipino
Filipino Français
Français Deutsch
Deutsch हिन्दी
हिन्दी Hmong
Hmong 한국어
한국어 Русский
Русский Español
Español தமிழ்
தமிழ் తెలుగు
తెలుగు Українська
Українська Tiếng Việt
Tiếng Việt